Uterine Anomalies
Uterine anomalies are structural abnormalities or malformations of the uterus, which may affect its size, shape, or position, and can potentially impact fertility and pregnancy outcomes.
There is evidence to suggest that there may be a relationship between uterine anomalies and endometriosis, although the exact nature of this relationship is not yet fully understood. Some studies have shown that women with certain uterine anomalies may have a higher risk of developing endometriosis, while other research has not found a significant association.
One theory is that certain uterine anomalies, such as a bicornuate uterus or a septate uterus, may create anatomical abnormalities that disrupt the normal flow of menstrual blood during menstruation. This altered flow may cause retrograde menstruation, which is when menstrual blood flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. Retrograde menstruation is thought to be a potential risk factor for the development of endometriosis, as it may allow endometrial tissue to implant and grow outside the uterus, leading to the formation of endometrial lesions.
It’s important to note that not all women with uterine anomalies develop endometriosis, and not all women with endometriosis have uterine anomalies. Other factors, such as genetic predisposition, hormonal imbalances, and immune system dysfunction, may also play a role in the development of endometriosis.
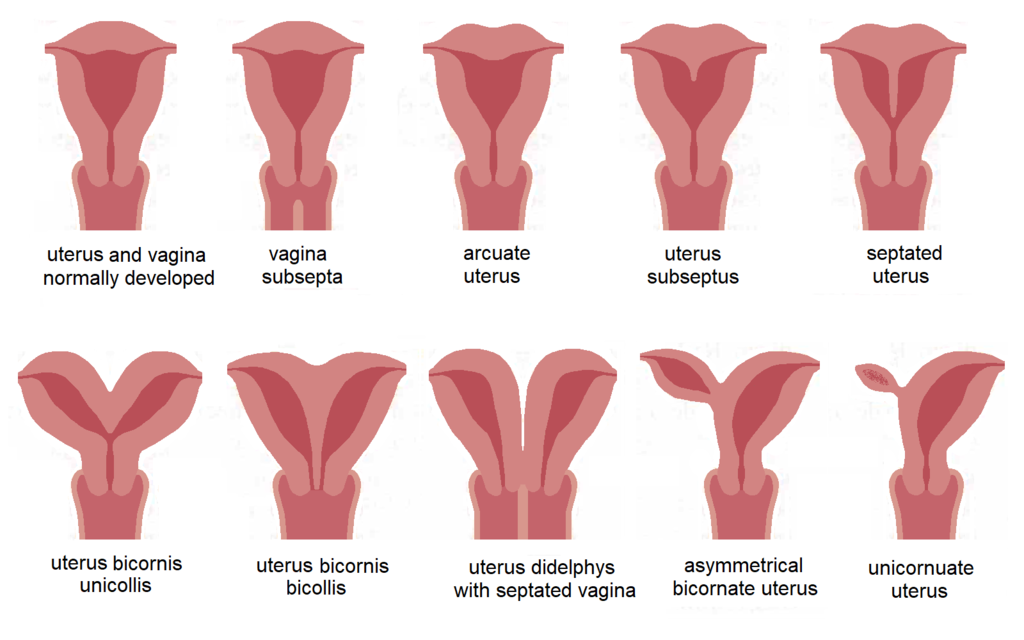
Uterine Malformation (Image source: Sciencia58, 2023)
Types of Uterine Anomalies
Uterine anomalies can be congenital, meaning they are present from birth, or acquired, meaning they develop later in life due to various factors.
There are different types of uterine anomalies, which can affect the size, shape, or position of the uterus. Some common types of uterine anomalies include:
Bicornuate uterus: A bicornuate uterus is characterized by a uterus that is divided into two separate “horns” with a deep indentation at the top. This anomaly occurs when the uterus fails to fuse properly during fetal development. It is estimated to occur in approximately 0.1-0.5% of the general female population.
Septate uterus: A septate uterus is characterized by a uterine cavity that is partially or completely divided by a septum, which is a wall of tissue. This anomaly occurs when the uterus fails to reabsorb the septum that forms during fetal development. It is estimated to occur in approximately 1-3% of women in the general population.
Unicornuate uterus: A unicornuate uterus is characterized by a uterus that is smaller in size and has only one horn. This anomaly occurs when one of the two ducts that form the uterus fails to develop properly during fetal development. It is estimated to occur in approximately 0.1-0.5% of women in the general population.
Didelphic uterus: A didelphic uterus is characterized by a uterus that is completely divided into two separate structures, each with its own cervix. This anomaly occurs when the two ducts that form the uterus fail to fuse properly during fetal development. It is estimated to occur in approximately 0.1-0.5% of women in the general population.
Arcuate uterus: An arcuate uterus is characterized by a small indentation or dip in the top of the uterus, but the overall shape of the uterus is relatively normal. This anomaly is considered to be a mild form of uterine anomaly. It is estimated to occur in approximately 10-15% of women in the general population.
Uterine anomalies can sometimes cause reproductive issues, such as infertility, recurrent miscarriages, and complications during pregnancy, as the abnormal shape or structure of the uterus may affect the implantation of a fertilized egg or the development of a fetus.
Müllerian Agenesis
Mullerian agenesis, also known as Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, is a rare congenital condition in females where the uterus and upper part of the vagina do not develop properly, while the external genitalia appear normal. This results in women with MRKH syndrome having a normal female karyotype (46,XX) but being born without a uterus or having an underdeveloped uterus.
According to the available literature, the estimated prevalence of Mullerian agenesis is approximately 1 in 4,000 to 1 in 5,000 female births.
MRKH syndrome is typically diagnosed during adolescence when a girl does not start menstruating, although the presence of normal secondary sexual characteristics (such as breast development and pubic hair) suggests that the ovaries are functional. Other signs and symptoms may include a shortened vagina, absence or underdevelopment of the cervix, and sometimes renal or skeletal anomalies.
The exact cause of MRKH syndrome is not yet fully understood, but it is believed to involve a combination of genetic and environmental factors. There is evidence to suggest that it may have a genetic component, as it can sometimes run in families, but the inheritance pattern is not always clear.
Effects of Uterine Anomalies
Uterine anomalies, which are structural abnormalities of the uterus, can have various effects on a woman’s reproductive health. They may cause infertility, recurrent miscarriages, pregnancy complications, pain and discomfort, obstetric complications during labor and delivery, abnormal fetal presentation, and increased risk of other gynecological conditions. The specific effects of uterine anomalies depend on the type, severity, and location of the anomaly, and can vary from mild to severe. It’s important to seek medical evaluation and management if you suspect you may have a uterine anomaly or are experiencing reproductive health issues.
Diagnosis of Uterine Anomalies
The diagnosis of uterine anomalies typically involves a combination of medical history, physical examination, imaging studies, and sometimes, specialized tests.
Here are some common methods used for diagnosing uterine anomalies:
- Medical history and physical examination: Your healthcare provider will likely take a detailed medical history, including any symptoms you may be experiencing, previous pregnancies, and menstrual history. A physical examination may also be performed to assess the shape, size, and position of the uterus.
- Imaging studies: Imaging studies are commonly used to visualize the structure of the uterus and identify any potential anomalies. These may include:
- Transvaginal ultrasound: This is a common imaging technique that uses a probe inserted into the vagina to obtain detailed images of the uterus and surrounding structures.
- Magnetic resonance imaging (MRI): MRI can provide more detailed and comprehensive images of the uterus, allowing for better visualization of uterine anomalies.
- Hysterosalpingography (HSG): HSG is a specialized X-ray procedure that involves injecting a contrast dye into the uterus and fallopian tubes to visualize their shape and outline. It can help detect abnormalities in the uterine cavity, such as septums or other structural anomalies.
- Hysteroscopy: Hysteroscopy is a minimally invasive procedure that involves inserting a thin, flexible tube with a camera (hysteroscope) through the cervix into the uterus to directly visualize the uterine cavity. It allows for direct visualization of the uterus and can help detect uterine anomalies.
- 3D ultrasound or saline infusion sonohysterography (SIS): These specialized ultrasound techniques can provide more detailed images of the uterine cavity and help detect uterine anomalies.
In some cases, further tests such as hormonal assessments, genetic testing, or additional imaging studies may be recommended based on the suspected type of uterine anomaly or associated conditions.
It’s important to note that the diagnosis of uterine anomalies requires specialized expertise and should be made by a qualified healthcare provider, such as a gynecologist, reproductive endocrinologist, or radiologist, who is experienced in diagnosing and managing uterine abnormalities.
Surgical Methods for the Treatment of Uterine Anomalies
The surgical methods for treating uterine anomalies depend on the specific type and severity of the anomaly, as well as the individual patient’s circumstances and reproductive goals. Here are some commonly used surgical methods for uterine anomalies:
Hysteroscopic Surgery
This minimally invasive surgical approach involves using a hysteroscope, which is a thin, flexible tube with a light and camera, to visualize and access the uterus through the cervix. Hysteroscopic surgery can be used to correct certain uterine anomalies that affect the inside of the uterus, such as septate uterus, submucosal fibroids, and uterine polyps. It involves removing or resecting the abnormal tissue or structure using specialized surgical instruments inserted through the hysteroscope.
It’s recommended to request an appointment with New York Gynecology Endometriosis (NYGE) to obtain an accurate estimate of the cost.
Laparoscopic Surgery
Laparoscopic surgery is a minimally invasive approach that involves making small incisions in the abdomen and using a laparoscope, which is a thin tube with a light and camera, to visualize and access the pelvic organs, including the uterus.
Laparoscopic surgery can be used to correct uterine anomalies that affect the outside of the uterus, such as bicornuate uterus, unicornuate uterus, or uterine didelphys. It may involve removing adhesions, dividing uterine septum, or reconstructing the uterus depending on the specific anomaly.
Robotic-Assisted Surgery
Robotic-assisted surgery is a type of minimally invasive surgery that uses a robotic system to assist the surgeon in performing the procedure. It can be used for certain complex cases of uterine anomalies, allowing for more precise and controlled movements. Robotic-assisted surgery may be used in cases where traditional laparoscopic surgery may be challenging or in cases where the surgeon has advanced expertise in robotic surgery.
Open Abdominal Surgery
In some cases, open abdominal surgery may be required for more complex uterine anomalies or in cases where laparoscopic or hysteroscopic approaches are not feasible or safe. Open abdominal surgery involves making a larger incision in the abdomen to access the uterus directly. This approach may be used for conditions such as large fibroids, extensive adhesions, or other complex uterine anomalies that require more extensive surgical intervention.
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries.

We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields