Rectal Endometriosis
Rectal endometriosis involves the growth of endometrial tissue outside the uterus, specifically affecting the rectal area, causing symptoms and requiring specialized treatment.
Rectal endometriosis is a condition in which endometrial tissue, which normally lines the inside of the uterus, is found outside the uterus and within or around the rectum. Endometriosis typically affects the pelvic organs, such as the ovaries, fallopian tubes, and pelvic peritoneum, but in rare cases, it can also invade the rectal area.
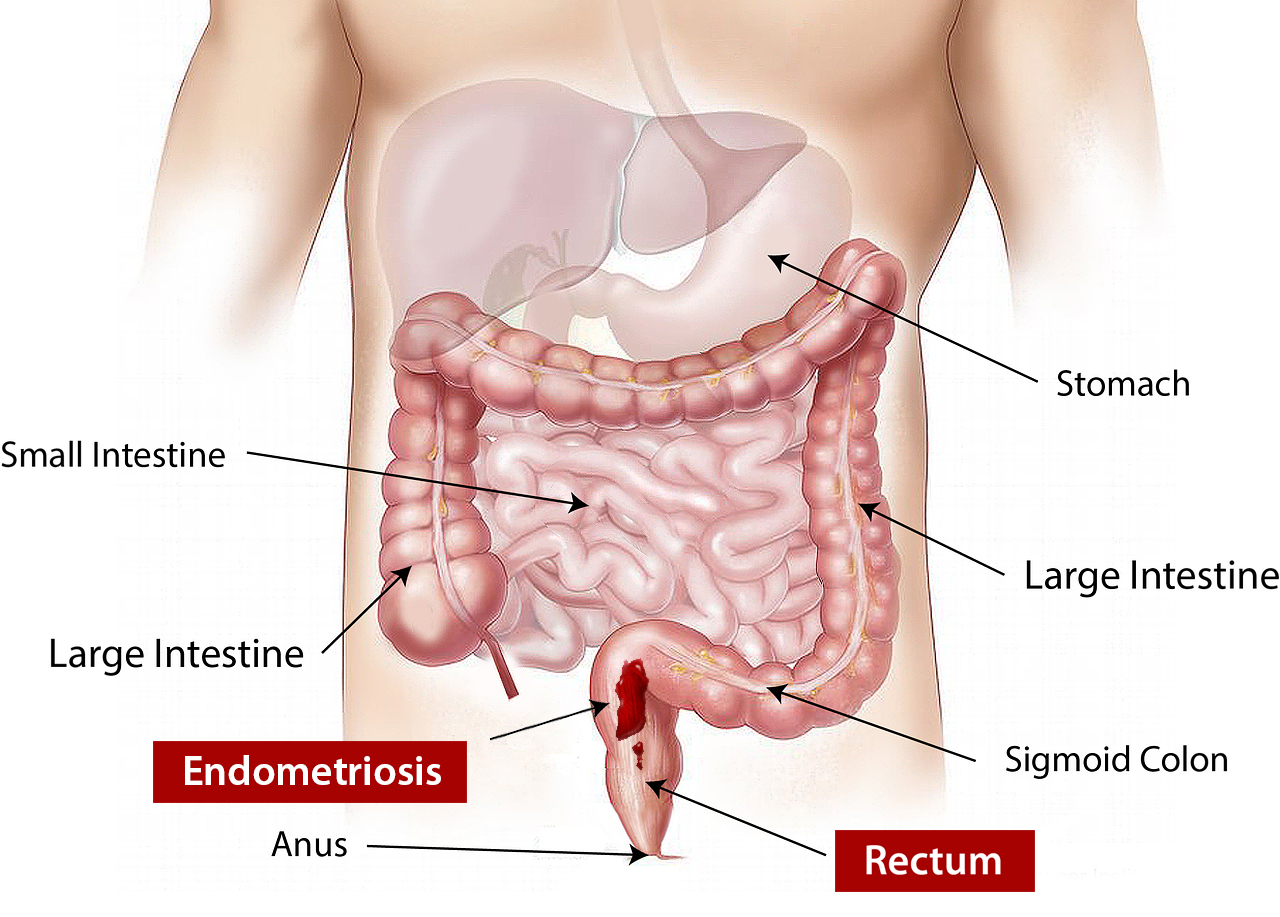
Endometriosis (Image source: Blausen Medical, 2014)
Causes of Rectal Endometriosis
The exact causes of rectal endometriosis are not fully understood, but there are several theories and factors that may contribute to its development. Here are some possible causes and contributing factors:
- Retrograde menstruation: Retrograde menstruation is a common theory for the development of endometriosis in general, including rectal endometriosis. It occurs when menstrual blood containing endometrial cells flows backward through the fallopian tubes and into the pelvic cavity instead of being expelled through the vagina. These endometrial cells can then implant and grow on various organs, including the rectum.
- Metaplasia: Metaplasia refers to the transformation of normal cells into endometrial-like cells. It is believed that certain cells in the pelvic region can undergo metaplasia and develop into endometrial tissue outside the uterus, including in the rectal area.
- Immune system dysfunction: It is thought that immune system dysfunction or alterations may contribute to the development of endometriosis. In a healthy immune system, immune cells would recognize and eliminate endometrial cells that have implanted outside the uterus. However, in individuals with endometriosis, the immune response may be impaired, allowing the endometrial cells to persist and grow.
- Genetic factors: There may be a genetic predisposition to endometriosis, including rectal endometriosis. If a close family member, such as a mother or sister, has endometriosis, the risk of developing the condition may be higher.
- Hormonal imbalances: Hormonal factors play a significant role in the growth and shedding of the endometrial tissue. It is believed that hormonal imbalances, particularly involving estrogen, may contribute to the development and progression of endometriosis. Estrogen can promote the growth of endometrial tissue outside the uterus, including in the rectal area.
It’s important to note that while these factors are associated with the development of endometriosis, they may not be the sole causes. The exact interplay of these factors and the individual’s susceptibility to endometriosis is still being researched.
Types of Rectal Endometriosis
Rectal endometriosis can be classified into different types based on the depth of infiltration and the extent of involvement. The classification helps in understanding the severity of the condition and determining appropriate treatment strategies. Here are the commonly recognized types of rectal endometriosis:
- Superficial endometriosis: Superficial rectal endometriosis refers to the presence of endometrial implants on the surface of the rectum or the peritoneum covering the rectum. In this type, the endometrial tissue does not penetrate deeply into the rectal wall.
- Nodular endometriosis: Nodular rectal endometriosis involves the formation of nodules or masses within the rectal wall. These nodules can be palpable during a rectal examination and may cause symptoms such as pain, bleeding, or bowel dysfunction.
- Deep infiltrating endometriosis (DIE): Deep infiltrating endometriosis is the most severe and extensive form of rectal endometriosis. In this type, the endometrial tissue penetrates deeply into the rectal wall and can extend beyond the rectum, involving nearby structures such as the vagina, bladder, or pelvic sidewalls. DIE can cause significant pain, bowel dysfunction, and other symptoms.
- Rectovaginal endometriosis: Rectovaginal endometriosis is a subtype of rectal endometriosis that specifically involves the area between the rectum and the vagina. It can result in the formation of nodules or adhesions that affect both the rectal and vaginal walls. This type often causes pain during intercourse and other symptoms related to both the rectum and vagina.
It’s important to note that these classifications are not mutually exclusive, and an individual may have a combination of different types of rectal endometriosis. The classification helps in determining the severity of the disease and guiding treatment decisions, including surgical approaches and the involvement of multidisciplinary teams.
Proper diagnosis and classification of rectal endometriosis are typically made through a combination of medical history review, physical examination, imaging studies (such as ultrasound or MRI), and sometimes a diagnostic laparoscopy.
Diagnosis of Rectal Endometriosis
The diagnosis of rectal endometriosis typically involves a comprehensive evaluation by a healthcare professional, often an endometriosis specialist or a team of specialists, to accurately assess the condition. Here are the main steps and methods involved in diagnosing rectal endometriosis:
- Medical history review: The healthcare professional will begin by discussing your symptoms, medical history, and any previous diagnoses or treatments related to endometriosis. They will ask specific questions about your bowel habits, rectal pain, bleeding, and other related symptoms.
- Physical examination: A pelvic examination may be performed to assess any abnormalities, tenderness, or masses in the pelvic region. A digital rectal examination may also be conducted to evaluate the rectum and detect any palpable nodules or abnormalities.
- Imaging studies: Imaging techniques can provide visual information about the pelvic organs and help identify any endometrial implants or structural abnormalities. The following imaging studies may be used:
- Ultrasound: Transvaginal or transrectal ultrasound can provide detailed images of the pelvic organs, including the rectum, and help identify endometrial implants or nodules.
- Magnetic Resonance Imaging (MRI): MRI can provide more detailed imaging of the pelvis and help visualize the extent of endometriosis, including the involvement of the rectum and surrounding structures.
- Colonoscopy or sigmoidoscopy: These procedures involve the insertion of a thin, flexible tube with a camera into the rectum and colon to directly visualize the lining and identify any endometrial implants or lesions. Biopsies may also be taken during these procedures to confirm the presence of endometrial tissue.
- Diagnostic laparoscopy: Laparoscopy is a surgical procedure performed under general anesthesia to directly visualize the pelvic organs and confirm the presence of endometriosis. During laparoscopy, a small incision is made near the navel, and a thin, lighted instrument called a laparoscope is inserted to examine the pelvic region. If rectal endometriosis is suspected, the surgeon may specifically focus on assessing the rectal area and obtain tissue samples (biopsies) for further analysis.
It’s important to note that a definitive diagnosis of rectal endometriosis often requires visualization and confirmation through laparoscopy, as other imaging techniques may not always provide a conclusive diagnosis. A multidisciplinary approach involving gynecologists, colorectal surgeons, and radiologists may be necessary for accurate diagnosis and treatment planning.
Difference Between Rectal and Bowel Endometriosis
Rectum and bowel endometriosis are both types of endometriosis that involve the gastrointestinal tract, but they refer to different areas within the digestive system.
Rectum endometriosis specifically refers to the presence of endometrial tissue within or around the rectum. The rectum is the final portion of the large intestine, located just above the anus. When endometrial tissue implants on or near the rectal wall, it can cause symptoms such as rectal pain, bleeding during bowel movements, and painful bowel movements.
On the other hand, bowel endometriosis refers to the involvement of the bowel as a whole, which includes the rectum as well as other parts of the intestine. Bowel endometriosis can affect different sections of the bowel, including the small intestine, large intestine (colon), and rectum. The extent of involvement can vary from superficial implants on the bowel surface to deep infiltration into the bowel wall.
The symptoms of bowel endometriosis can be similar to those of rectum endometriosis and may include rectal pain, bleeding during bowel movements, painful bowel movements, constipation, diarrhea, and abdominal pain. In some cases, bowel endometriosis can lead to bowel obstruction or strictures, which can cause severe abdominal pain and affect normal bowel movements.
Surgical Methods for Rectal Endometriosis Treatment
Surgical intervention is often required to effectively treat rectal endometriosis. Here are some surgical methods commonly used for rectal endometriosis treatment:
Rectal Laparoscopic Excision
Rectal laparoscopic excision, also known as rectal shaving or rectal nodule resection, is a surgical procedure performed to remove endometriotic lesions affecting the rectum. It is a minimally invasive approach that offers several advantages over open surgery, including smaller incisions, reduced scarring, shorter recovery time, and less post-operative pain.
It’s worth noting that rectal laparoscopic excision is typically performed by gynecological surgeons or colorectal surgeons who have expertise in treating endometriosis. The specific details of the surgery may vary depending on the extent and location of the rectal endometriosis, as well as the surgeon’s preferences and techniques.
The average cost for laparoscopic excision of endometriosis (including rectal involvement) in the United States can range from approximately $8,000 to $20,000 or more. This estimate includes the surgeon’s fees, anesthesia charges, hospital facility fees, pre-operative and post-operative care, and any necessary follow-up visits.
It is recommended to request an appointment with New York Gynecology Endometriosis (NYGE) to obtain an accurate estimate of the cost.
Robotic-Assisted Laparoscopy
Rectal robotic-assisted laparoscopy, also known as robotic-assisted rectal surgery, is a surgical technique that combines laparoscopic surgery with robotic technology to perform rectal procedures. It involves using the da Vinci Surgical System or a similar robotic platform to enhance the surgeon’s precision, control, and visualization during the procedure.
The use of robotic technology in rectal surgery offers several potential advantages, including improved visualization, enhanced precision, and reduced risk of complications. However, it’s important to note that not all rectal surgeries require robotic assistance, and the decision to use robotic-assisted laparoscopy is based on the surgeon’s judgment and the patient’s specific condition.
Bowel Resection
Bowel resection is a surgical procedure that may be performed to treat rectal endometriosis when the disease has deeply infiltrated the rectal wall or involves a significant portion of the bowel. It involves removing the affected segment of the rectum and rejoining the healthy ends of the bowel. Bowel resection aims to eliminate the endometriotic lesions and restore normal bowel function.
It’s important to note that bowel resection is a major surgical procedure and carries potential risks and complications, including bleeding, infection, anastomotic leakage, bowel obstruction, and the need for a permanent colostomy in rare cases. The decision to perform bowel resection for rectal endometriosis is typically made based on factors such as the severity of the disease, symptoms, and the patient’s desire for fertility preservation.
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries.

We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage.
Surgeries are typically covered by health insurance. However, the extent of coverage can vary depending on the specific insurance plan and policy. Some insurance plans may cover a broad range of surgical procedures, including both elective and necessary surgeries, while others may have limitations or exclusions for certain procedures.
In some cases, certain insurance plans or programs may fully cover the cost of surgery, leaving the patient with no financial responsibility.
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields