Stage 2 Endometriosis
Stage 2 endometriosis involves the presence of minimal to mild implants of endometrial tissue outside the uterus and pelvic lining.
Stage 2 endometriosis is a classification within the four-stage system used to assess the severity of endometriosis, a chronic medical condition affecting individuals with female reproductive organs. In this stage, the condition is considered to be at a relatively moderate level of progression. It is characterized by the presence of minimal to mild implants of endometrial tissue outside the uterus and pelvic lining.
These implants, also known as lesions or growths, may be found on various pelvic organs and tissues, such as the ovaries, fallopian tubes, and the peritoneum (the lining of the abdominal cavity). Despite their presence outside the uterus, these endometrial tissue growths continue to respond to hormonal changes in the menstrual cycle, causing them to shed and bleed.
However, unlike more advanced stages of endometriosis, stage 2 is associated with fewer and smaller implants, and there may be less overall tissue involvement in the pelvic region. As with all stages of endometriosis, symptoms can vary widely, but they may include pelvic pain, painful menstrual periods, pain during intercourse, and infertility. Early diagnosis and appropriate management are crucial in order to alleviate symptoms and improve the quality of life for individuals with stage 2 endometriosis.
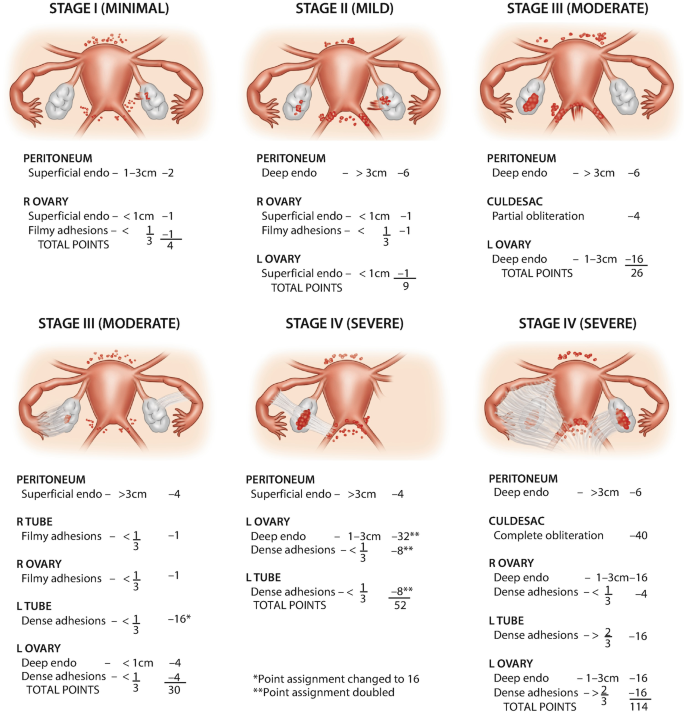
Stages of Endometriosis (Image source: Springer Nature Switzerland AG, 2022)
Symptoms of Stage 2 Endometriosis
Stage 2 endometriosis, characterized by minimal to mild implants of endometrial tissue outside the uterus and pelvic lining, can present with a range of symptoms that may vary from person to person. Common symptoms of stage 2 endometriosis may include:
- Pelvic Pain: Women with stage 2 endometriosis often experience pelvic discomfort or pain, which can be intermittent or chronic. The pain might be dull, sharp, or cramp-like and can worsen during menstruation, intercourse, or bowel movements.
- Painful Menstruation: Menstrual periods may be accompanied by more intense and prolonged cramps, often starting a few days before the period and lasting throughout its duration.
- Painful Intercourse: Pain or discomfort during sexual intercourse, known as dyspareunia, is a common symptom. It may be felt deep within the pelvis or lower abdomen.
- Gastrointestinal Symptoms: Some individuals might experience gastrointestinal issues such as bloating, constipation, diarrhea, or nausea, particularly around the time of their menstrual cycle.
- Fatigue: Chronic pain and other symptoms can contribute to feelings of fatigue and general tiredness.
- Infertility: Stage 2 endometriosis can affect fertility, as the abnormal tissue growths might interfere with the function of the ovaries, fallopian tubes, or uterus.
- Irregular Bleeding: Women with stage 2 endometriosis might experience irregular menstrual bleeding, spotting between periods, or heavy bleeding.
It’s worth highlighting that the intensity of symptoms is not always directly linked to the stage of endometriosis; individuals with stage 2 endometriosis can encounter varying degrees of symptom severity, ranging from significant discomfort to minimal effects.
If you suspect you may have endometriosis or are experiencing any symptoms of concern, it’s essential to request an appointment with New York Gynecology Endometriosis (NYGE) to seek medical advice and evaluation.
Life-threatening Complications in Stage 2 Endometriosis
While stage 2 endometriosis is generally considered to have a lower risk of life-threatening complications compared to more advanced stages, there are still potential concerns that individuals should be aware of. One notable risk is the potential impact on fertility. Even at this stage, endometriosis can lead to scarring and adhesions that may affect the reproductive organs, potentially leading to difficulties in conceiving and carrying a pregnancy to term.
Another concern is the possibility of severe and chronic pelvic pain. While not life-threatening in itself, this pain can significantly diminish an individual’s quality of life, potentially leading to mental health challenges and a decreased ability to engage in daily activities. Additionally, there is a small chance that endometrial tissue could attach to vital structures such as the intestines or bladder, potentially causing complications such as bowel obstruction or urinary issues. While these risks are relatively uncommon at stage 2, it’s important for individuals with endometriosis to stay informed, seek medical guidance, and explore appropriate treatment options to manage their condition and minimize potential complications.
Diagnosis of Stage 2 Endometriosis
Diagnosing stage 2 endometriosis involves:
- Clinical Assessment: Your healthcare provider will gather your medical history and discuss your symptoms, focusing on menstrual patterns, pelvic pain, and other relevant information.
- Physical Examination: A pelvic exam may be conducted to check for tender areas, masses, or other signs of endometriosis.
- Imaging: Ultrasound or MRI scans may be used to visualize pelvic structures, helping identify possible endometriosis-related abnormalities.
- Laparoscopy: Considered the definitive diagnostic method, a minimally invasive surgical procedure (laparoscopy) allows direct visualization of pelvic organs, enabling the doctor to identify and evaluate endometriosis lesions. Biopsies can be taken for confirmation.
Early diagnosis and intervention can lead to more effective management and improved quality of life for individuals with endometriosis.
Surgical Treatment for Stage 2 Endometriosis
A common surgical treatment for stage 2 endometriosis is laparoscopic excision or removal of endometrial tissue growths. This minimally invasive procedure aims to alleviate symptoms, improve quality of life, and potentially enhance fertility.
Laparoscopy
Laparoscopy is a widely employed treatment for stage 2 endometriosis, a condition characterized by minimal to mild implants of endometrial tissue outside the uterus and pelvic lining. This minimally invasive surgical procedure serves a dual purpose of diagnosis and intervention.
During laparoscopy, a small incision is made near the navel, through which a thin tube with a camera (laparoscope) is inserted. The surgeon utilizes real-time visual guidance to examine the pelvic region, confirming the presence and extent of endometrial tissue growths.Upon identification, the surgeon can delicately excise or ablate these growths, removing abnormal tissue, adhesions, and cysts as needed. By addressing these tissue implants, laparoscopy aims to alleviate symptoms such as pelvic pain, painful menstruation, and discomfort during intercourse that often accompany stage 2 endometriosis. Its minimally invasive nature generally leads to quicker recovery times, reduced postoperative pain, and decreased scarring compared to traditional open surgery.
Following laparoscopy, a tailored treatment plan, potentially including pain management and hormonal therapies, may be recommended to manage symptoms and prevent recurrence, ensuring improved quality of life for individuals with stage 2 endometriosis.
According to Healthcare Bluebook, the cost of laparoscopic excision of endometriosis can vary depending on the location, healthcare provider, and type of insurance. On average, the cost of the procedure can range from $4,000 to $15,000. It’s important to note that these are estimated costs and may not reflect the actual cost you may incur.
To obtain an accurate cost estimate, it is advisable to request an appointment with New York Gynecology Endometriosis (NYGE).
Excision or Ablation
When addressing stage 2 endometriosis, two primary surgical options are excision and ablation, both aimed at removing or destroying endometrial tissue growths outside the uterus. Excision involves the meticulous removal of these growths, along with any associated scar tissue or adhesions. This method aims to fully eliminate the abnormal tissue, potentially providing more comprehensive relief from symptoms like pelvic pain, while also reducing the risk of recurrence. Excision is often preferred when the goal is to achieve long-term symptom management and enhance fertility, as it addresses the underlying tissue involvement.
In contrast, ablation employs techniques like heat or laser to destroy the endometrial tissue growths. While less invasive than excision, ablation may not completely eliminate all abnormal tissue, potentially leaving behind microscopic implants.
Robotic Surgery
Robotic surgery is emerging as an advanced and minimally invasive option for treating stage 2 endometriosis, characterized by minimal to mild endometrial tissue growths outside the uterus and pelvic lining. This technique involves the use of robotic-assisted surgical systems, where a surgeon controls robotic arms equipped with surgical instruments to perform precise and intricate procedures. Robotic surgery offers enhanced dexterity, visualization, and maneuverability, making it well-suited for addressing endometriosis lesions with precision.
During robotic surgery for stage 2 endometriosis, small incisions are made to insert robotic arms and a high-definition camera into the abdomen. The surgeon controls the robotic arms from a console, guiding them to remove endometrial tissue growths and address any adhesions or scar tissue. This minimally invasive approach often leads to reduced postoperative pain, shorter hospital stays, and quicker recovery compared to traditional open surgery. Robotic surgery’s increased precision can aid in sparing healthy tissue and minimizing potential damage to surrounding structures, which is particularly advantageous when treating stage 2 endometriosis to alleviate symptoms like pelvic pain, painful periods, and fertility issues.
- Dr Pankaj Singhal performed more than 10,000 robotic gynecologic, endometriosis and cancer surgeries.
- He is known for taking on the most challenging surgery cases that other doctors or centers turn away.
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries.
We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage.
Surgeries are typically covered by health insurance. However, the extent of coverage can vary depending on the specific insurance plan and policy. Some insurance plans may cover a broad range of surgical procedures, including both elective and necessary surgeries, while others may have limitations or exclusions for certain procedures.
In some cases, certain insurance plans or programs may fully cover the cost of surgery, leaving the patient with no financial responsibility.
Hear From Our Clients

Leslie Patriarco
NYGE has truly changed my life. I had previous endometriosis surgery costing 15k by one of the well known providers out there in NYC which was a 6 hour drive for me to only require surgery again 2 years later.
The doctors are excellent and knowledgeable from their excision abilities and understanding of the disease, to their surgical skills, to their patient care. I am 6 weeks out from surgery and they still will check in on me and answer any and all questions that I have.
I am so beyond grateful to have found them.

Josie Beck
Dr Singhal is an Amazing and Excellent Doctor! He explains things thoroughly and was kind and has an excellent bedside manner! He reassured and comforted me about the procedure and what my options would be.
Took the time to answer all my questions and concerns. His Staff is excellent as well. Returning calls, and always there to answer questions. There was never a long wait to see him.
He is truly one of the Best Surgeons and Doctors! I highly recommend him!!

Merari Mejia
Dr. Singhal and Dr. McLean are very thorough and knowledgeable surgeons. They set clear expectations for my two surgeries. I was operated for stage 4 endometriosis by Dr. Singhal and Dr. McLean.
The surgical incisions are very small and barely noticeable. The surgeries relieved the GI symptoms I was experiencing, such as painful bowel movements, bloating, and distention.
I would highly recommend them to anyone needing their expertise.
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields