Ovarian Cysts and Pelvic Mass
Ovarian cysts are fluid-filled sacs that form on or within the ovaries, which are part of the female reproductive system, and a pelvic mass refers to an abnormal lump or swelling located in the pelvic area, including the lower abdomen and pelvis.
The menstrual cycle is a monthly hormonal cycle that occurs in reproductive-age females and involves the release of an egg from the ovary (ovulation), preparation of the uterus for potential pregnancy, and shedding of the uterine lining (menstruation) if pregnancy does not occur.
During the menstrual cycle, ovarian cysts can form as part of the normal physiological process. These cysts are known as functional ovarian cysts and are the most common type of ovarian cysts. Functional ovarian cysts can occur during different stages of the menstrual cycle:
- Follicular cysts: These cysts form when the follicle, which is a fluid-filled sac in the ovary that contains an immature egg, does not release the egg during ovulation. Instead, the follicle continues to grow and becomes a cyst. Follicular cysts are more likely to occur in the early part of the menstrual cycle, before ovulation.
- Corpus luteum cysts: These cysts form after ovulation, when the follicle releases the egg and transforms into a structure called the corpus luteum. The corpus luteum produces hormones that support a potential pregnancy. If the corpus luteum does not regress as it should, it can become a cyst.
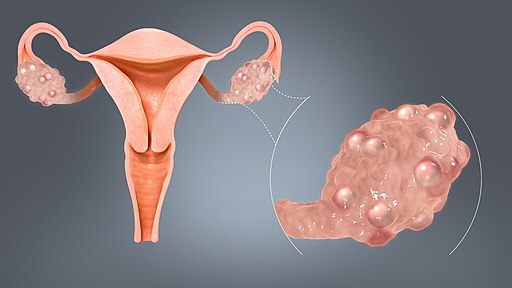
Ovarian Cysts (Image source: Blausen Medical, 2014)
Most functional ovarian cysts are benign and resolve on their own without treatment, typically within a few menstrual cycles. They often do not cause any symptoms and are discovered incidentally during routine pelvic examinations or imaging tests. However, in some cases, functional ovarian cysts can grow in size and cause pain or discomfort, or in rare cases, lead to complications such as cyst rupture or torsion (twisting), which can be serious and require medical attention.
What Makes the Identification of Ovarian Cysts Challenging?
Ovarian cysts can be challenging to identify due to several reasons, including the lack of symptoms in many cases, common symptoms that may overlap with other conditions, variability in size and appearance of cysts on imaging tests, overlapping features with other conditions, limitations of imaging tests, and hormonal changes and menstrual cycle variability that can affect cyst size and characteristics.
These factors can make it difficult to definitively identify ovarian cysts, and further evaluation, repeat imaging, or additional diagnostic tests may be necessary for accurate diagnosis and appropriate management. It’s important to consult with a qualified healthcare professional for proper evaluation and management of ovarian cysts.
Causes of Ovarian Cysts
Ovarian cysts can have various causes, including:
Follicular cysts: These cysts form when the sacs in the ovary that contain the eggs (follicles) do not release the egg and instead continue to grow, resulting in a cyst.
Corpus luteum cysts: These cysts form after the release of an egg when the follicle that released the egg does not dissolve as it normally would but instead seals off and accumulates fluid, leading to a cyst.
Endometriomas: These cysts form when endometrial tissue, which normally lines the uterus, implants and grows on the ovary, resulting in the formation of cysts.
Cystadenomas: These cysts develop from the ovarian tissue and are usually filled with a watery or mucous-like fluid. They can be benign (non-cancerous) or malignant (cancerous).
Polycystic ovary syndrome (PCOS): PCOS is a hormonal disorder that can result in the formation of multiple small cysts on the ovaries due to follicles that do not mature and develop into eggs.
Dermoid cysts: These cysts are usually benign and form from cells that produce eggs. They can contain various types of tissues, such as hair, skin, and teeth.
Other factors: Ovarian cysts can also be caused by hormonal imbalances, ovarian tumors, infections, or other underlying medical conditions.
It’s important to note that not all ovarian cysts cause symptoms or require treatment. Some cysts may resolve on their own without intervention, while others may require medical management, especially if they cause symptoms, are large, or are suspected to be malignant.
Classifications of Ovarian Cysts
Ovarian cysts can be classified into several types based on their characteristics, including:
Functional cysts: These are the most common type of ovarian cysts and are usually related to the normal hormonal changes that occur during the menstrual cycle. Functional cysts can be further classified into two subtypes:
Follicular cysts: These cysts form when the follicles in the ovary do not release the egg and instead continue to grow, resulting in the formation of a cyst.
Corpus luteum cysts: These cysts form after the release of an egg when the follicle that released the egg does not dissolve as it normally would but instead seals off and accumulates fluid, leading to the formation of a cyst.
Dermoid cysts: These cysts are usually benign and can contain various types of tissues, such as hair, skin, teeth, and other types of tissues. Dermoid cysts are typically present from birth and can grow slowly over time.
Endometriomas: Also known as chocolate cysts, these cysts form when endometrial tissue, which normally lines the uterus, implants and grows on the ovary, resulting in the formation of cysts.
Cystadenomas: These cysts develop from the ovarian tissue and are usually filled with a watery or mucous-like fluid. They can be benign (non-cancerous) or malignant (cancerous).
Polycystic ovary syndrome (PCOS): PCOS is a hormonal disorder that can result in the formation of multiple small cysts on the ovaries due to follicles that do not mature and develop into eggs.
Others: Other types of ovarian cysts can include paraovarian cysts (cysts near the ovary), cystic teratomas (benign tumors that can contain various types of tissues), and functional ovarian cysts associated with pregnancy.
Are Ovarian Cysts and Pelvic Masses the Same Thing?
Ovarian cysts and pelvic masses are related but distinct concepts.
Ovarian cysts refer to fluid-filled sacs that form on the ovaries. They can have various causes, such as functional cysts related to the normal hormonal changes during the menstrual cycle, dermoid cysts containing various types of tissues, endometriomas formed by endometrial tissue, and others. Ovarian cysts are typically benign, but in some cases, they can be malignant (cancerous). Ovarian cysts are usually small and may not cause symptoms, but they can grow larger and cause pain, discomfort, or other symptoms. Diagnosis is typically done through imaging tests, such as ultrasound, and treatment depends on the type, size, and symptoms associated with the cyst.
On the other hand, pelvic masses refer to any abnormal growth or lump that is present in the pelvic region, which is the lower part of the abdomen located between the hip bones. Pelvic masses can have various origins, including the ovaries, uterus, fallopian tubes, bladder, or other pelvic organs. Pelvic masses can be benign or malignant, and they can have different causes, such as tumors, cysts, or other abnormalities. Diagnosis of pelvic masses typically involves a thorough evaluation by a healthcare professional, including physical examination, imaging tests, and sometimes biopsies. Treatment options for pelvic masses depend on the underlying cause, size, location, and whether they are benign or malignant.
Ovarian cysts and pelvic masses share some similarities, as they both refer to abnormal growths or lumps in the pelvic region. Here are some similarities between ovarian cysts and pelvic masses:
- Location: Both ovarian cysts and pelvic masses are located in the pelvic region, which is the lower part of the abdomen between the hip bones.
- Benign or malignant: Both ovarian cysts and pelvic masses can be either benign (non-cancerous) or malignant (cancerous), although benign ovarian cysts are more common.
- Symptoms: Both ovarian cysts and pelvic masses can cause symptoms, such as pain, discomfort, bloating, changes in menstrual cycle, or urinary symptoms, depending on their size, location, and characteristics.
It’s important to note that while ovarian cysts are a type of pelvic mass, not all pelvic masses are ovarian cysts, as pelvic masses can have various causes and origins beyond the ovaries.
How Can Endometriosis Lead to Ovarian Cyst Development?
Endometriosis can lead to ovarian cyst development through a process called endometrioma formation or “chocolate cyst” formation. Endometriosis is a condition where the tissue that normally lines the uterus (endometrium) grows outside of the uterus, commonly on the ovaries, fallopian tubes, and other pelvic organs.
In cases of ovarian endometriosis, endometrial tissue can implant and grow on the surface of the ovary. Over time, this endometrial tissue can form a cyst that becomes filled with old blood, which gives it a characteristic dark, chocolate-like appearance on imaging studies. These cysts are called endometriomas or “chocolate cysts.”
As endometrial tissue continues to bleed and shed during a woman’s menstrual cycles, the endometriomas can grow larger and cause pain, discomfort, and other symptoms. The presence of endometriomas can also interfere with normal ovarian function, potentially leading to fertility issues in some cases.
Diagnosis of Ovarian Cysts
Diagnosis of ovarian cysts typically involves a combination of medical history, physical examination, and imaging studies. Here are some common steps involved in diagnosing ovarian cysts:
- Medical history: Your healthcare provider will take a detailed medical history, including any symptoms you may be experiencing, such as pelvic pain, bloating, changes in menstrual cycle, or other related symptoms. They will also inquire about any previous history of ovarian cysts or other relevant medical conditions.
- Physical examination: Your healthcare provider may perform a physical examination, including a pelvic examination, to check for any palpable masses or tenderness in the pelvic region. They may also assess other signs and symptoms that may be associated with ovarian cysts.
- Imaging studies: Imaging studies are commonly used to visualize the ovaries and confirm the presence of ovarian cysts. Transvaginal ultrasound is often the first-line imaging modality used, as it provides detailed images of the ovaries and can help identify the size, location, and characteristics of the cysts. Other imaging studies, such as abdominal ultrasound, CT scan, or MRI, may be used in certain cases to further evaluate the cysts or assess for any complications.
- Blood tests: Blood tests, such as CA-125 levels, may be ordered to help evaluate ovarian cysts, especially if there are concerns about the possibility of ovarian cancer. However, CA-125 levels alone are not definitive for diagnosing ovarian cysts and may require further evaluation.
- Other tests: In some cases, additional tests, such as hormonal tests or biopsies, may be ordered to further evaluate ovarian cysts, especially if there are concerns about the type or nature of the cysts.
- Clinical judgment: Diagnosis of ovarian cysts may also involve the clinical judgment of a qualified healthcare provider, who will consider the results of the medical history, physical examination, imaging studies, and other tests in the context of the patient’s overall health and individual circumstances.
What is Ovarian Torsion?
Ovarian torsion is a medical condition where the ovary becomes twisted on its own blood vessels, disrupting the blood supply to the ovary. This can cause severe pain and potentially lead to damage or death of the ovarian tissue if not promptly treated. Ovarian torsion is a medical emergency and requires immediate medical attention.
The treatment for ovarian torsion typically involves surgical intervention to untwist the ovary and restore blood flow. Depending on the severity of the torsion and the condition of the affected ovary, the surgical approach may vary.
Surgical Methods for the Treatment of Ovarian Cysts
Surgical treatment for ovarian cysts may be considered in cases where the cyst is large, causing severe symptoms, suspected to be cancerous, or if there are concerns about the possibility of ovarian torsion (twisting) or rupture. The surgical approach will depend on various factors, including the size and type of the cyst, the age and overall health of the patient, and the surgeon’s judgment.
The surgical treatment options for ovarian cysts may include:
Laparoscopy
Laparoscopy is a minimally invasive surgical technique that involves making small incisions in the abdomen and inserting specialized surgical instruments, including a laparoscope (a thin, flexible tube with a light and camera) to visualize and access the ovaries. The surgeon can then use the instruments to remove or drain the ovarian cyst while preserving the surrounding ovarian tissue. Laparoscopy is associated with shorter hospital stays, quicker recovery times, and less scarring compared to traditional open surgery.
As of 2023, according to the Healthcare Bluebook, the estimated fair price for a laparoscopy procedure in the United States ranges from approximately $3,000 to $10,000, depending on the complexity of the procedure and the specific location. This estimated fair price typically includes the surgeon’s fees, anesthesia fees, and facility fees, but may not include additional costs such as pre-operative tests, medications, and post-operative care.
It’s recommended to request an appointment with New York Gynecology Endometriosis (NYGE) to obtain an accurate estimate of the cost.
Laparotomy
Laparotomy is a more invasive surgical approach that involves making a larger abdominal incision to access the ovaries directly. This approach may be used in cases where the cyst is too large or complex to be safely removed or drained through laparoscopy, or if there are concerns about the possibility of ovarian torsion or cancer. Laparotomy may be associated with longer hospital stays, slower recovery times, and increased scarring compared to laparoscopy.
As of 2023, according to the Healthcare Bluebook, the estimated fair price for a laparotomy procedure in the United States ranges from approximately $6,000 to $25,000 or more, depending on the complexity of the procedure and the specific location.
Oophorectomy
In some cases, if the ovarian cyst is associated with a high risk of malignancy or if there are concerns about the viability of the ovary, the surgeon may need to remove the entire ovary (oophorectomy) along with the cyst. This may be done through either laparoscopy or laparotomy, depending on the circumstances.
As of 2023, according to the Healthcare Bluebook, the estimated fair price for an oophorectomy procedure in the United States ranges from approximately $4,000 to $20,000 or more.
References
Benign ovarian cysts. (April 5, 2023). Johns Hopkins University. https://www.hopkinsmedicine.org/health/conditions-and-diseases/benign-ovarian-cysts
Healthcare Bluebook. (2023). https://www.healthcarebluebook.com/explore-home/
Ovarian cysts: Frequently asked questions. (July 2021). The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/ovarian-cysts
Ovarian cysts: Overview. (March 28, 2019). National Library of Medicine – National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK539572/
Ovarian cysts treatment. (October 3, 2018) National Health Service (NHS) of England. https://www.nhs.uk/conditions/ovarian-cyst/treatment/
Ovarian torsion. (July 13, 2021) Yale Medicine. https://www.yalemedicine.org/conditions/ovarian-torsion
Practical approach to MRI of female pelvic masses. (June 2014). American Journal of Roentgenology. https://www.ajronline.org/doi/10.2214/AJR.13.12023
The management of ovarian cysts in postmenopausal women. (July 2016). Royal College of Obstetricians and Gynaecologists. https://www.rcog.org.uk/media/4v3ncfib/gtg_34.pdf
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries.

We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields