Laparoscopic Oophorectomy
Laparoscopic oophorectomy is a minimally invasive surgical procedure that involves the removal of one or both ovaries through small incisions in the abdomen.
Oophorectomy, whether unilateral or bilateral, is a surgical procedure involving the removal of one or both ovaries, often combined with the removal of the fallopian tubes (salpingo-oophorectomy) or performed as part of a total hysterectomy (removal of the uterus).
Dr. Pankaj Singhal, the chief surgeon of New York Gynecology Endometriosis, is a highly experienced gynecological surgeon with more than 25 years of expertise, renowned for his pioneering work in laparoscopic oophorectomy surgery, prioritizing minimal invasiveness.
We have consistently led the way in delivering the appropriate approach to oophorectomy, emphasizing that the removal of one or both ovaries should be considered as a final option, prioritizing alternative treatments whenever possible.
It is common for doctors to remove both ovaries during a hysterectomy for non-cancerous conditions to prevent future ovarian cancer or other problems that may need more surgery. In 2009, about 78% of women aged 45 to 64 who had a hysterectomy also had both ovaries removed, and approximately 300,000 preventive oophorectomies are performed each year in the USA. (Parker et al., 2009)
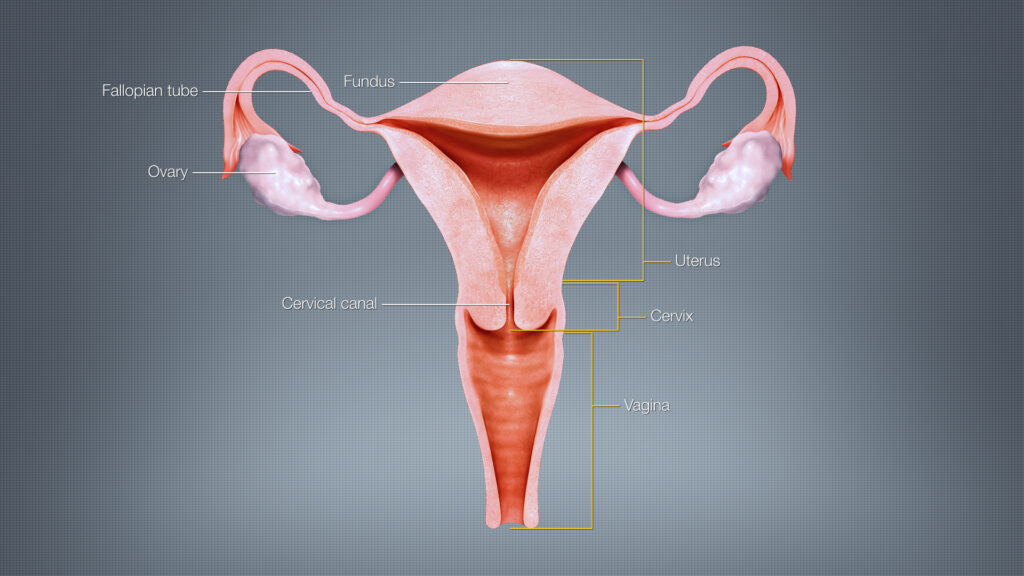
Uterus (Image source: ShareAlike 4.0 International)
What is the Function of the Uterus?
The ovaries are a pair of reproductive organs in females that serve several important functions.
Production of eggs: The ovaries are responsible for producing and releasing eggs (ova) during the menstrual cycle. Each ovary contains thousands of immature eggs, and usually, one egg is released each month during ovulation.
Hormone production: The ovaries produce hormones such as estrogen and progesterone. These hormones are crucial for the development and regulation of the female reproductive system, including the menstrual cycle, maintenance of pregnancy, and development of secondary sexual characteristics.
Reproductive health: The ovaries play a vital role in female fertility. They are responsible for the maturation and release of eggs, which are necessary for fertilization by sperm and the initiation of pregnancy.
It’s important to note that the removal of the ovaries has significant implications for a woman’s reproductive health and hormonal balance, which may lead to menopause symptoms and potential long-term health effects. Therefore, the decision to undergo oophorectomy should be carefully discussed with an experienced gynecologic surgeon like Dr. Pankaj Singhal, to weigh the potential benefits and risks.
Types of Oophorectomy
There are two main types of oophorectomy based on the number of ovaries being removed:
- Unilateral Oophorectomy: This procedure involves the removal of one ovary while leaving the other intact. It may be performed when there are specific indications, such as the presence of an ovarian tumor or cyst on one side, while the other ovary is healthy.
- Bilateral Oophorectomy: In bilateral oophorectomy, both ovaries are surgically removed. This procedure may be performed for various reasons, including the treatment or prevention of ovarian cancer, management of certain gynecological conditions, or as a part of a total hysterectomy (removal of the uterus along with both ovaries).
- Salpingo-oophorectomy is a surgical procedure that involves the removal of both the fallopian tubes (salpingectomy) and the ovaries (oophorectomy).
- Bilateral salpingo-oophorectomy is a surgical procedure in which both fallopian tubes and ovaries are removed. It is sometimes referred to as BSO (bilateral salpingo-oophorectomy).
Reasons for Oophorectomy
There are several reasons why oophorectomy, the removal of one or both ovaries, may be recommended. These reasons include:
Ovarian cancer: Oophorectomy is often performed as part of the treatment for ovarian cancer. Removing the affected ovary or ovaries can help eliminate the cancerous cells and prevent the spread of the disease.
Prevention of ovarian cancer: Women with a high risk of developing ovarian cancer, such as those with a family history of the disease or specific genetic mutations (e.g., BRCA1 or BRCA2), may choose to undergo preventive oophorectomy. By removing the ovaries, the risk of developing ovarian cancer in the future can be significantly reduced.
Non-cancerous ovarian conditions: Oophorectomy may be recommended for the treatment of non-cancerous conditions affecting the ovaries, such as large ovarian cysts, endometriosis, or benign tumors. Removing the affected ovary or ovaries can alleviate symptoms and prevent further complications.
Hormone-related disorders: In certain cases, oophorectomy may be performed to manage hormone-related disorders. For example, in women with polycystic ovary syndrome (PCOS) who do not respond to other treatments, removing the ovaries may help regulate hormone levels and improve symptoms.
Oophorectomy as Endometriosis Treatment
Oophorectomy may be considered as a treatment option for endometriosis in certain cases. Some reasons why oophorectomy may be recommended for endometriosis include:
Severe or refractory endometriosis: If endometriosis is severe and causing significant pain or other symptoms that do not respond to other treatment options, oophorectomy may be considered. Removing the ovaries, which are the primary source of estrogen, can help reduce estrogen levels and suppress the growth of endometrial tissue.
Endometriomas: Endometriomas are cysts that form on the ovaries due to endometriosis. If these cysts are large, causing pain, or interfering with fertility, oophorectomy may be recommended to remove the affected ovary and the associated endometriomas.
Hormone suppression: Oophorectomy is a more aggressive form of hormonal suppression for endometriosis. By removing the ovaries, which produce estrogen, the overall estrogen levels in the body are significantly reduced, helping to manage the symptoms and progression of endometriosis.
It’s important to note that oophorectomy is typically considered a last resort for endometriosis treatment, reserved for cases where other interventions have been ineffective or the condition is severe.
Effects of Oophorectomy
Oophorectomy, the surgical removal of one or both ovaries, can have significant effects on a woman’s body and health. Here are some common effects of oophorectomy:
- Menopause: Oophorectomy results in an abrupt hormonal change, leading to menopause if both ovaries are removed. Menopause symptoms such as hot flashes, night sweats, vaginal dryness, mood changes, and changes in libido may occur. These symptoms can vary in severity and duration.
- Hormonal imbalance: Removal of the ovaries disrupts the normal production of estrogen and progesterone, leading to hormonal imbalance. This can affect bone health, cardiovascular health, and overall well-being.
- Infertility: If both ovaries are removed, it will result in permanent infertility, as the eggs are no longer produced. This is an important consideration for women who wish to have children in the future.
- Sexual health changes: Oophorectomy can impact sexual health due to the hormonal changes and potential loss of libido. Vaginal dryness and decreased sexual desire may occur, affecting sexual function and satisfaction.
- Long-term health effects: Studies suggest that oophorectomy before natural menopause may increase the risk of certain conditions, such as osteoporosis, heart disease, cognitive decline, and overall mortality. Hormone replacement therapy (HRT) may be recommended to manage these risks in some cases.
It’s crucial for women considering a oophorectomy to have a thorough discussion with New York Gynecology Endometriosis (NYGE) to fully understand the implications specific to their situation and explore alternative treatments or procedures when appropriate.
Common Complications that Can Arise After Laparoscopic Oophorectomy
While laparoscopic oophorectomy is generally considered a safe procedure, there are potential complications that can arise. Some common complications include:
Infection: Infection at the site of incisions or within the pelvic region can occur after surgery. This risk can be minimized with proper sterile techniques and post-operative care.
Bleeding: Excessive bleeding during or after the surgery is a possible complication. In most cases, bleeding can be controlled during the procedure, but occasionally, it may require additional intervention.
Damage to surrounding organs: During the surgery, there is a slight risk of unintentional damage to nearby organs, such as the bladder, intestines, or blood vessels. Surgeons take precautions to minimize this risk, but it can still occur in rare cases.
Adverse reactions to anesthesia: Some individuals may experience allergic reactions or other complications related to the administration of anesthesia.
Blood clots: There is a risk of developing blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism) after surgery. Measures such as early mobilization, leg exercises, and blood thinning medications are typically used to reduce this risk.
Scar tissue formation: Laparoscopic oophorectomy involves making small incisions, but in some cases, scar tissue may develop around the incision sites. This can lead to discomfort or adhesions (bands of scar tissue) that can cause pain or affect organ function.
Persistent or new symptoms: While oophorectomy is performed to alleviate symptoms or treat a specific condition, there is a possibility that some symptoms may persist or new symptoms may arise after the surgery.
What Benefits Does Oophorectomy Offer in the Treatment of Endometriosis?
Endometriosis has no current cure, and oophorectomy is typically considered a final option after all other treatments have failed, especially if the patient does not wish to preserve fertility. While oophorectomy can help reduce symptoms such as pain, there is still a possibility of symptom recurrence.
According to Dr. Mortlock (2022), “Overall, studies have estimated that 1 in 76 women are at risk of developing ovarian cancer in their lifetime, and having endometriosis increases this slightly to 1 in 55, indicating a still relatively low overall risk.” If there is a confirmed or suspected presence of ovarian cancer, a specialized gynecologic surgeon will make an informed treatment decision that often includes oophorectomy.
As a last-resort treatment for endometriosis, oophorectomy can provide pain relief by inducing “surgical menopause” and ceasing menstrual cycles. However, if endometriosis lesions or scar tissue remain in the pelvis without surgical removal, there is a chance that pain may persist even after oophorectomy, particularly if hormone replacement therapy is used. Therefore, the decision to pursue oophorectomy should involve thorough discussion between the patient and surgeon.
Laparoscopic Oophorectomy
The most common surgical technique used for oophorectomy is laparoscopic oophorectomy. In this procedure, small incisions are made in the abdomen, and a laparoscope (a thin, lighted instrument with a camera) is inserted to provide a view of the pelvic organs. The surgeon then uses specialized instruments to carefully remove the ovaries through the small incisions.
Laparoscopic oophorectomy is a minimally invasive technique that offers several advantages over traditional open surgery. It typically results in less post-operative pain, smaller incisions, faster recovery, and reduced scarring. Additionally, it carries a lower risk of complications such as infection and bleeding compared to open surgery.
In some cases, open surgery (laparotomy) may be necessary, especially if the ovaries are large or if there are other underlying medical conditions that make laparoscopic surgery more challenging or risky. Open oophorectomy involves a larger incision in the abdomen, providing the surgeon with direct access to the ovaries for their removal.
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries.

Frequently Asked Questions
It’s important to request an appointment with New York Gynecology Endometriosis (NYGE) to discuss specific concerns, questions, and individual circumstances regarding oophorectomy.
Is oophorectomy performed alone or with other procedures?
Oophorectomy can be performed alone or in combination with other procedures, such as hysterectomy (removal of the uterus) or salpingectomy (removal of fallopian tubes).
What are the potential risks and complications of oophorectomy?
Oophorectomy, like any surgery, carries risks such as infection, bleeding, damage to surrounding organs, adverse reactions to anesthesia, and the formation of scar tissue. It also has implications for reproductive health, hormonal balance, and long-term health effects. Discussing these risks with a healthcare provider is essential.
How do you recover after oophorectomy?
Following the surgery, you will be transferred to a recovery room where you will remain until the effects of the general anesthesia diminish. The length of your hospital stay will depend on the type of procedure, ranging from a few hours for minimally invasive techniques to a few days for laparotomy.
In general, you can resume your daily activities on the same day of the surgery. However, it is advisable to avoid lifting heavy objects or engaging in vigorous exercise for a few weeks. Detailed instructions will be provided regarding the cleaning and maintenance of the incision sites.
Will I go into menopause after oophorectomy?
If both ovaries are removed, oophorectomy will induce menopause. If one ovary is removed, menopause may not occur immediately, but the remaining ovary may still undergo changes in hormonal function.
Can hormone replacement therapy (HRT) be used after oophorectomy?
In some cases, hormone replacement therapy (HRT) may be recommended to manage menopause symptoms and hormonal imbalances that occur after oophorectomy. HRT should be discussed with a healthcare provider to determine if it is appropriate for individual circumstances.
Can I still have children after oophorectomy?
If both ovaries are removed, oophorectomy will result in permanent infertility as the eggs are no longer produced. If fertility preservation is a concern, it should be discussed with a healthcare provider before undergoing oophorectomy.
How long is the recovery period after oophorectomy?
The recovery period can vary depending on the surgical technique and individual factors. Generally, it may take a few weeks to several months to fully recover. It is important to follow post-operative instructions and attend follow-up appointments for proper healing and monitoring.
How much is the cost of oophorectomy?
The cost of oophorectomy in the United States can vary widely depending on various factors such as the specific procedure performed, the surgeon’s fees, the hospital or surgical facility charges, geographical location, and any additional services or tests required.
Without insurance, the total cost for oophorectomy can range from several thousand dollars to tens of thousands of dollars. This includes pre-operative consultations, surgical fees, anesthesia costs, hospital or surgical facility fees, pathology tests, and post-operative care.
However, it’s important to note that insurance coverage and individual healthcare plans can greatly impact the out-of-pocket expenses for the procedure. Health insurance may cover a significant portion of the cost, including hospitalization, surgeon fees, and associated medical services.
It’s recommended to request an appointment with New York Gynecology Endometriosis (NYGE) to obtain an accurate estimate of the cost.
We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields