Laparoscopic Hysterectomy
A hysterectomy is a surgical procedure that involves the removal of the uterus, the reproductive organ in females where the fetus develops during pregnancy.
A laparoscopic hysterectomy is a minimally invasive surgical procedure that uses small incisions and specialized instruments to remove the uterus and, in some cases, other reproductive organs, typically resulting in less pain, faster recovery, and smaller scars compared to traditional open surgery.
Dr. Pankaj Singhal, the chief surgeon of New York Gynecology Endometriosis, is a highly experienced gynecological surgeon with more than 25 years of expertise, renowned for his pioneering work in laparoscopic hysterectomy surgery, prioritizing minimal invasiveness.
We have consistently led the way in delivering the appropriate approach to hysterectomies, emphasizing that the removal of the uterus should be considered as a final option, prioritizing alternative treatments whenever possible.
In the United States, hysterectomy ranks as the second most commonly performed surgical procedure for women of reproductive age, following cesarean section, with approximately 600,000 hysterectomies conducted each year and an estimated 20 million women in the country having undergone the procedure (Keshavarz et al., 1999).
Hysterectomy is sometimes considered as a treatment option for endometriosis, a condition in which the tissue that normally lines the inside of the uterus grows outside of it. However, it’s important to note that hysterectomy alone is not a definitive cure for endometriosis.
In cases where endometriosis is severe and causing significant pain or other complications, a hysterectomy may be recommended as part of a comprehensive treatment plan. The goal of a hysterectomy in endometriosis cases is to remove the uterus, which eliminates the possibility of uterine-related symptoms and can potentially reduce the spread or growth of endometrial tissue.
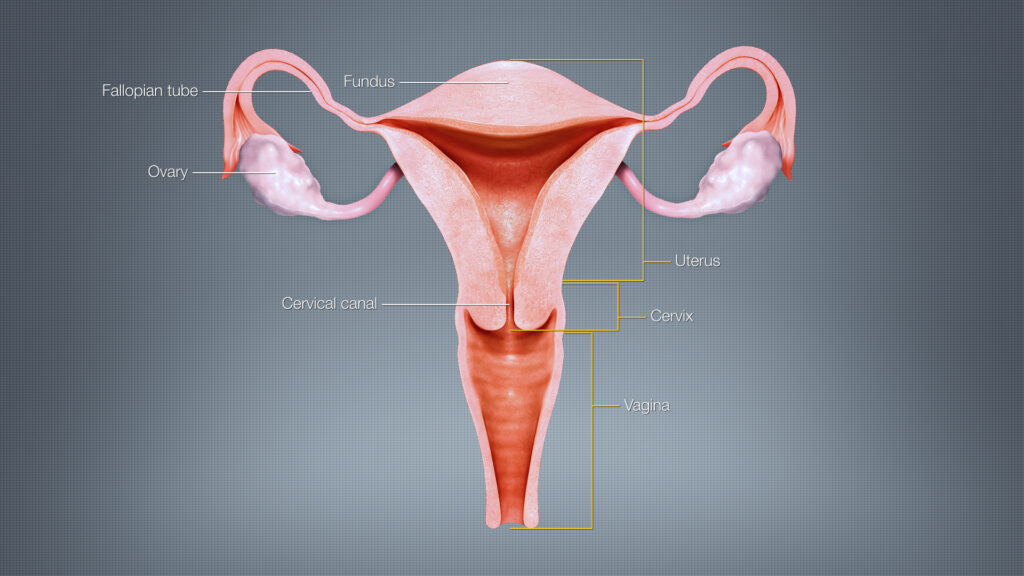
Uterus (Image source: ShareAlike 4.0 International)
What is the Function of the Uterus?
The uterus, also known as the womb, is a vital reproductive organ in females. Its main functions include:
- Fetal Development: The uterus is where a fertilized egg implants and develops into a fetus during pregnancy. It provides a nourishing environment and supports the growth and development of the embryo into a baby.
- Menstruation: The uterus plays a role in the menstrual cycle. Each month, the inner lining of the uterus, called the endometrium, thickens in preparation for a potential pregnancy. If pregnancy does not occur, the uterus sheds this lining through menstruation.
- Hormone Production: The uterus produces various hormones that regulate the menstrual cycle and support pregnancy. These hormones include progesterone, estrogen, and prostaglandins, which play important roles in the preparation of the uterus for pregnancy and the maintenance of pregnancy.
- Pelvic Organ Support: The uterus helps provide support to other pelvic organs, including the bladder and rectum, through its position and ligament attachments.
It’s important to note that while the uterus is essential for pregnancy and menstruation, its removal (hysterectomy) does not generally have significant adverse effects on overall health or hormone production, especially when the ovaries are preserved.
Types of Hysterectomy
It is crucial to recognize that hysterectomy does not guarantee a complete cure for endometriosis, and often multiple surgeries may be necessary with the possibility of incomplete pain relief.
There are different types of hysterectomies available, depending on the extent of organ removal. These include:
Total Hysterectomy: In a total hysterectomy, both the uterus and the cervix are removed. This is the most common type of hysterectomy.
Partial or Subtotal Hysterectomy: In a partial or subtotal hysterectomy, only the upper part of the uterus is removed, while the cervix is left intact.
Radical Hysterectomy: A radical hysterectomy involves the removal of the uterus, cervix, upper part of the vagina, and supporting tissues. This type of hysterectomy is typically performed for gynecologic cancers.
Total Hysterectomy with Bilateral Salpingo-Oophorectomy: In this procedure, in addition to the uterus and cervix, both the fallopian tubes and ovaries are removed. This results in surgical menopause if the woman has not reached menopause naturally.
Effects of Hysterectomy
Hysterectomy, the surgical removal of the uterus, can have several implications for women. Here are some key implications to consider:
Infertility: Hysterectomy leads to the loss of reproductive capability, as the uterus is essential for pregnancy. If the ovaries are also removed during the procedure, it can result in surgical menopause and the cessation of natural hormone production.
Menstruation and Hormonal Changes: Hysterectomy eliminates menstruation since the uterus, where the menstrual lining develops, is removed. However, if the ovaries are preserved, hormonal changes may be minimal. If the ovaries are removed, hormonal fluctuations and menopausal symptoms can occur.
Impact on Sexual Function: Hysterectomy may have an impact on sexual function for some women. While the procedure itself doesn’t directly affect sexual desire, the physical and emotional changes associated with the surgery or resulting hormonal changes may affect sexual well-being. It’s important to have open communication with your healthcare provider and address any concerns.
Relief from Gynecological Conditions: Hysterectomy can provide relief from certain gynecological conditions such as uterine fibroids, endometriosis, chronic pelvic pain, and abnormal uterine bleeding. Removing the source of these conditions can improve quality of life for many women.
Emotional and Psychological Impact: Hysterectomy can have emotional and psychological implications, particularly if a woman has a strong attachment to her reproductive organs or if the surgery was performed due to underlying health concerns. It’s important to seek emotional support, if needed, and address any feelings or concerns that may arise.
It’s crucial for women considering a hysterectomy to have a thorough discussion with New York Gynecology Endometriosis (NYGE) to fully understand the implications specific to their situation and explore alternative treatments or procedures when appropriate.
Common Complications that Can Arise After Laparoscopic Hysterectomy
While laparoscopic hysterectomy is generally considered a safe surgical procedure, there are potential complications that can occur after the surgery. It’s important to note that not all individuals will experience these complications, and the likelihood and severity can vary depending on factors such as individual health, the specific circumstances of the surgery, and the skill of the surgeon. Some common complications that can occur after a laparoscopic hysterectomy include:
- Infection: Surgical site infections or infections of the urinary tract can occur after a laparoscopic hysterectomy. Signs of infection may include fever, redness, swelling, increased pain, or discharge from the incision sites.
- Bleeding: While minimal bleeding is expected after a laparoscopic hysterectomy, excessive or prolonged bleeding may occur and require medical attention.
- Prolapse: Prolapse refers to the descent or displacement of pelvic organs, such as the bladder, rectum, or vaginal walls, into the vaginal canal. It can occur as a potential complication after the removal of the uterus during a hysterectomy. The risk of prolapse can vary depending on various factors, including the type of hysterectomy performed, the presence of pre-existing pelvic floor weakness, and individual factors.
- Blood clots: There is a relatively rare risk of developing blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism) after any surgery, including laparoscopic hysterectomy. Factors such as prolonged immobility, obesity, smoking, or a personal or family history of blood clots can increase this risk.
- Urinary or bowel problems: Some individuals may experience temporary changes in bladder or bowel function after a laparoscopic hysterectomy. These can include difficulty emptying the bladder, urinary urgency or incontinence, or constipation.
- Shoulder pain: After laparoscopic surgery, some individuals may experience shoulder pain due to the carbon dioxide gas used to inflate the abdomen during the procedure. This pain is typically temporary and resolves within a few days.
- Adverse reaction to anesthesia: Rarely, individuals may experience complications related to anesthesia, such as allergic reactions or breathing difficulties.
Benefits of Laparoscopic Hysterectomy
Laparoscopic hysterectomy, being a minimally invasive surgical procedure, has several implications that differ from traditional open hysterectomy. Here are some key implications of laparoscopic hysterectomy:
Smaller Incisions and Reduced Scarring: Laparoscopic hysterectomy involves making small incisions, typically less than an inch in size, compared to a large abdominal incision in open surgery. As a result, there is generally less scarring and a lower risk of post-surgical complications related to wound healing.
Reduced Blood Loss and Pain: Laparoscopic hysterectomy is associated with reduced blood loss during surgery, which may lead to a lower need for blood transfusions. Additionally, patients often experience less post-operative pain compared to open surgery, leading to a more comfortable recovery period.
Shorter Hospital Stay: With laparoscopic hysterectomy, the hospital stay is typically shorter compared to open surgery. Patients may be able to go home on the same day or within a few days, depending on individual factors and the complexity of the procedure.
Faster Recovery: Due to the minimally invasive nature of laparoscopic hysterectomy, the recovery time is generally faster compared to open surgery. Patients may resume their normal activities and return to work sooner, although the specific timeline varies depending on individual factors and the extent of the surgery.
Reduced Risk of Infection: Laparoscopic hysterectomy minimizes the risk of surgical site infections since the incisions are smaller, resulting in fewer openings for potential infection. This is particularly advantageous for patients with a higher risk of surgical complications, such as those with compromised immune systems.
Potential for Preserving Ovaries: Laparoscopic hysterectomy offers the possibility of preserving the ovaries, depending on the underlying condition and the surgeon’s assessment. Preserving the ovaries allows women to continue producing hormones, potentially avoiding the immediate onset of menopause and its associated symptoms.
It’s important to note that while laparoscopic hysterectomy offers several advantages, it may not be suitable for all patients or conditions. The appropriateness of this procedure should be determined through a comprehensive evaluation with NYGE, taking into account individual medical needs and factors.
- What is Laparoscopic Hysterectomy?
- Functions of Uterus
- Types of Hysterectomy
- - Total Hysterectomy
- - Partial or Subtotal Hysterectomy
- - Radical Hysterectomy
- - Total Hysterectomy with Bilateral Salpingo-Oophorectomy
- Effects of Hysterectomy
- Common Complications of Laparoscopic Hysterectomy
- Benefits of Laparoscopic Hysterectomy
Types of Laparoscopic Hysterectomies
There are several types of laparoscopic hysterectomies, each with its own approach and extent of organ removal.
Laparoscopic Total Hysterectomy
Laparoscopic total hysterectomy can be considered as a treatment option for endometriosis. This minimally invasive surgical procedure involves using small incisions and specialized instruments to remove the uterus, including the cervix, with the assistance of a laparoscope (a camera).
In cases where endometriosis is severe and causing significant pain or other complications, laparoscopic total hysterectomy may be recommended as part of a comprehensive treatment plan. By removing the uterus, it eliminates the possibility of uterine-related symptoms and may help alleviate pain associated with endometriosis.
However, it’s important to note that laparoscopic total hysterectomy alone does not remove all endometrial tissue, as endometriosis can also affect other pelvic organs. Therefore, additional procedures, such as excision or ablation of endometrial implants or removal of affected organs like the ovaries or fallopian tubes, may be necessary to address endometriosis comprehensively.
Partial or Subtotal Hysterectomy
Partial or subtotal hysterectomy, also known as supracervical hysterectomy, can be considered as a treatment option for endometriosis in certain cases. In this procedure, only the upper part of the uterus is removed, while the cervix is left intact.
For women with endometriosis who have not responded well to other treatments and whose symptoms primarily involve the uterus, a partial hysterectomy may be considered. It can help alleviate symptoms such as pain, heavy menstrual bleeding, or other uterine-related issues.
It’s important to note that while laparoscopic partial hysterectomy can provide relief from symptoms related to the uterus, it does not address endometriosis affecting other pelvic organs such as the ovaries, fallopian tubes, or surrounding tissues. Therefore, additional treatments or procedures may be necessary to comprehensively manage endometriosis.
Laparoscopic Radical Hysterectomy
A laparoscopic radical hysterectomy is a surgical procedure performed to treat gynecologic cancers, particularly cervical cancer or endometrial cancer. In this procedure, the surgeon uses laparoscopic techniques to remove the uterus, cervix, upper part of the vagina, and surrounding tissues, including lymph nodes if necessary.
Laparoscopic radical hysterectomy offers several benefits compared to traditional open surgery, including smaller incisions, reduced blood loss, shorter hospital stays, faster recovery times, and potentially less post-operative pain. The laparoscope, a thin tube with a camera, allows the surgeon to visualize and operate inside the abdomen with precision.
Total Hysterectomy with Bilateral Salpingo-Oophorectomy
Total hysterectomy with bilateral salpingo-oophorectomy (removal of the uterus, fallopian tubes, and ovaries) can be considered as a treatment option for endometriosis in certain cases. This surgical procedure aims to remove the sources of estrogen production and eliminate endometriosis-associated pain and symptoms.
Total hysterectomy with bilateral salpingo-oophorectomy may be recommended for women with severe endometriosis that has not responded to other treatments, or for those who have completed their childbearing years and want to eliminate the possibility of future endometriosis-related issues.
It’s important to note that this procedure induces surgical menopause since the ovaries, which produce hormones, are removed. Surgical menopause can lead to hormonal changes and potential symptoms such as hot flashes, mood swings, and bone density changes. Hormone replacement therapy (HRT) may be prescribed to manage these symptoms and minimize the long-term effects of estrogen loss.
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries.

We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage.
Surgeries are typically covered by health insurance. However, the extent of coverage can vary depending on the specific insurance plan and policy. Some insurance plans may cover a broad range of surgical procedures, including both elective and necessary surgeries, while others may have limitations or exclusions for certain procedures.
In some cases, certain insurance plans or programs may fully cover the cost of surgery, leaving the patient with no financial responsibility.
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields