Frozen Pelvis in Endometriosis
Frozen pelvis refers to severe pelvic adhesions resulting from the abnormal growth of endometrial tissue outside the uterus, causing significant pain, organ fixation, and limited mobility.
To be considered a frozen pelvis, specific criteria include the presence of dense and extensive adhesions that result in complete or near-complete immobility and fixation of pelvic organs, significant distortion of pelvic anatomy, and severe limitations in normal pelvic function and mobility.
- “Frozen pelvis” is not an officially recognized medical term, but it refers to an unofficial condition where the organs in the pelvis, such as the rectum, bladder, ureters, uterus, and even the large and small bowel, are tightly adhered to each other due to deeply infiltrating endometriosis.
- The tubes, ovaries, and pelvic ligaments can also be affected. The criterion for diagnosing “deeply infiltrating endometriosis” (referred to as DIE) is the presence of solid endometriosis that extends more than 5 mm into the pelvic floor, which typically forms the foundation of the adherent organs.
- These densely adhered organs develop nerves within the adhesions, contributing to pain that originates from the inflammatory process of endometriosis.
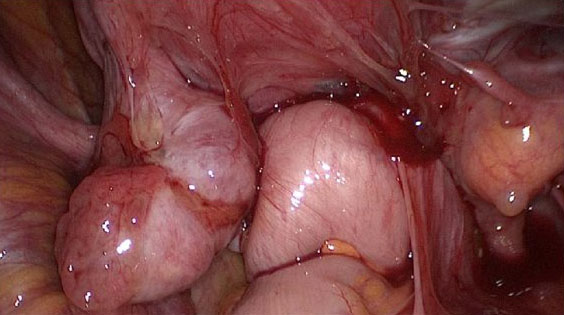
Frozen pelvis with invisible deep endometriosis
(bilateral ovary, left cardinal ligament, ureter left, anterior wall of the rectum)
(Image source: Human Reproduction Open, 2020)
How Common is Frozen Pelvis in Endometriosis?
The exact prevalence of frozen pelvis in endometriosis is challenging to determine due to variations in diagnostic criteria, study populations, and methodologies. However, frozen pelvis is considered a relatively uncommon but severe complication of endometriosis. It occurs when the pelvic organs become densely adhered to each other due to extensive endometriotic involvement and the formation of scar tissue (adhesions).
Frozen pelvis is more commonly observed in advanced stages of endometriosis, particularly when deeply infiltrating endometriosis (DIE) affects the pelvic organs such as the rectum, bladder, uterus, and bowel. It can also involve the fallopian tubes, ovaries, and pelvic ligaments.
While specific prevalence rates are lacking, estimates suggest that frozen pelvis occurs in a minority of individuals with endometriosis, ranging from around 5% to 15% of cases. It is important to note that these numbers may vary based on the population studied and the diagnostic criteria used.
Early detection and appropriate management of endometriosis are crucial to minimize the risk of developing a frozen pelvis. Regular medical follow-up, effective pain management, and timely intervention can help prevent the progression of endometriosis to severe adhesions and frozen pelvis.
Symptoms of Frozen Pelvis
The symptoms of frozen pelvis can vary depending on the underlying cause and the specific organs involved. However, common symptoms associated with frozen pelvis include:
- Chronic pelvic pain: Persistent and severe pain in the pelvic region is a hallmark symptom of frozen pelvis. The pain may be dull, aching, or sharp in nature and can be constant or intermittent.
- Limited mobility: Frozen pelvis can result in restricted movement and reduced flexibility in the pelvic area. This can lead to difficulty in bending, twisting, or performing normal daily activities.
- Pain during sexual intercourse: Adhesions and organ fixation in the pelvis can cause pain and discomfort during sexual intercourse, known as dyspareunia.
- Bowel and bladder dysfunction: Adhesions involving the bowel and bladder can lead to symptoms such as constipation, diarrhea, bloating, urinary urgency, or difficulty emptying the bladder.
- Infertility or reproductive issues: In some cases, frozen pelvis can impact fertility by obstructing or distorting the fallopian tubes, affecting egg release, or impairing implantation.
- Gastrointestinal symptoms: Depending on the extent and location of adhesions, symptoms like abdominal pain, bloating, nausea, and changes in bowel habits may be present.
It’s important to note that these symptoms are not exclusive to frozen pelvis and can be associated with other pelvic conditions as well. If you are experiencing any of these symptoms, it is advisable to request an appointment with New York Gynecology Endometriosis (NYGE) for a comprehensive evaluation and appropriate diagnosis.
Classification of Frozen Pelvis
This classification provides additional information about the location and distribution of adhesions within the pelvis. The most commonly used classification based on patterns is the American Society for Reproductive Medicine (ASRM) classification. The ASRM classification system divides frozen pelvis into four patterns:
- Pattern I (Uterosacral ligament involvement): This pattern involves adhesions primarily affecting the uterosacral ligaments, which are fibrous bands that attach the uterus to the sacrum (the triangular bone at the base of the spine). Adhesions in this pattern can cause fixation of the uterus and limited mobility of the pelvic structures.
- Pattern II (Posterior cul-de-sac involvement): In this pattern, adhesions primarily involve the posterior cul-de-sac, also known as the Pouch of Douglas. The cul-de-sac is the space between the uterus and rectum. Adhesions in this pattern can lead to the uterus and other pelvic structures being fixed in a posterior position.
- Pattern III (Anterior cul-de-sac involvement): This pattern involves adhesions primarily affecting the anterior cul-de-sac, which is the space between the uterus and bladder. Adhesions in this pattern can cause fixation of the uterus and other pelvic structures in an anterior position.
- Pattern IV (Diffuse involvement): In this pattern, adhesions are widespread and involve multiple areas of the pelvis, including the uterosacral ligaments, posterior cul-de-sac, and anterior cul-de-sac. The adhesions in this pattern are often dense and can cause significant distortion and fixation of pelvic structures.
The pattern classification provides information about the specific areas affected by adhesions and can help guide surgical planning and treatment approaches. It assists in determining the complexity of the frozen pelvis and the potential challenges that may be encountered during surgical intervention. However, it’s important to note that the patterns may overlap or coexist in some cases, and individual variations can exist within each pattern.

Deep Endometriosis
(Image source: Complete Anatomy, as cited in Human Reproduction Open, 2020)
Which healthcare professionals are qualified to perform surgery for a frozen pelvis?
Surgery for a frozen pelvis should ideally be performed by a skilled and experienced surgical team that includes healthcare professionals with expertise in the management of endometriosis and complex pelvic conditions. The specific specialists involved may vary depending on the extent and nature of the frozen pelvis, as well as the individual patient’s needs. Here are some healthcare professionals who may be involved in the surgical management of a frozen pelvis:
- Gynecologist: Gynecologists with advanced training and experience in the surgical treatment of endometriosis are often the primary surgeons involved in addressing a frozen pelvis. They specialize in the diagnosis and management of conditions affecting the female reproductive system, including endometriosis.
- Colorectal surgeon: If the frozen pelvis involves significant bowel involvement or adhesions, a colorectal surgeon may be consulted or directly involved in the surgical procedure. They specialize in the diagnosis and treatment of conditions affecting the colon, rectum, and anus.
- Urologist: In cases where the frozen pelvis affects the bladder, ureters, or other urinary structures, a urologist may be involved in the surgical management. Urologists specialize in the diagnosis and treatment of urinary system disorders.
- Multidisciplinary team: Depending on the complexity of the frozen pelvis and associated conditions, a multidisciplinary team may be formed, involving gynecologists, colorectal surgeons, urologists, and other specialists. This collaborative approach ensures comprehensive evaluation, surgical planning, and coordinated care.
It is crucial to seek treatment from healthcare professionals or medical centers like New York Gynecology Endometriosis (NYGE) with experience in managing frozen pelvis and the associated conditions. They can provide an accurate diagnosis, evaluate the extent of the condition, and recommend appropriate surgical interventions based on individual circumstances.
Surgical Treatment of Frozen Pelvis Causes by Endometriosis
The surgical treatment of frozen pelvis caused by endometriosis typically involves a comprehensive approach aimed at relieving adhesions, restoring normal pelvic anatomy and function, and alleviating associated symptoms. The specific surgical procedures performed may vary depending on the extent and severity of the adhesions and the individual patient’s circumstances.
Here are some common surgical treatment options:
Laparoscopic surgery
Laparoscopy is a minimally invasive surgical technique commonly used for the treatment of endometriosis-related frozen pelvis. It involves making small incisions in the abdomen through which a thin, flexible camera (laparoscope) and surgical instruments are inserted. The surgeon can visualize the pelvic organs and carefully dissect and remove the adhesions.
According to the Healthcare Bluebook, the cost of laparoscopic excision surgery ranges from $6,440 to $20,380, with an average cost of $13,790 in the United States. However, it’s important to note that the actual cost may vary depending on several factors such as the location of the facility, the experience of the surgeon, and the complexity of the procedure. It’s also worth checking with your insurance provider to see what portion of the cost will be covered.
To obtain an accurate cost estimate, it is advisable to make an appointment with New York Gynecology Endometriosis (NYGE).
Adhesiolysis
Adhesiolysis refers to the surgical removal or separation of adhesions. During this procedure, the surgeon carefully separates the adhered organs, restoring their mobility and function. Various techniques, such as sharp dissection, electrocautery, or laser therapy, may be utilized to release the adhesions.
Excision of Endometriosis Lesions
If endometriosis lesions are present within the adhesions, the surgeon may perform excision or removal of these abnormal growths. Excision aims to completely remove the endometriotic tissue while preserving the healthy surrounding tissue.
Organ-specific Procedures
In cases where specific pelvic organs, such as the bowel, bladder, ureters, or uterus, are significantly involved in the frozen pelvis, additional procedures may be required. These may include bowel resection or re-anastomosis, bladder repair, ureteral re-implantation, or even hysterectomy (removal of the uterus) if necessary.
Multidisciplinary Approach
Depending on the complexity of the frozen pelvis and associated symptoms, a multidisciplinary approach involving gynecologists, colorectal surgeons, urologists, or other specialists may be required to optimize surgical outcomes.
- Dr Pankaj Singhal performed more than 10,000 robotic gynecologic, endometriosis and cancer surgeries.
- Known for taking on the most challenging surgery cases that other doctors/centers turn away.
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries.
We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage.
Surgeries are typically covered by health insurance. However, the extent of coverage can vary depending on the specific insurance plan and policy. Some insurance plans may cover a broad range of surgical procedures, including both elective and necessary surgeries, while others may have limitations or exclusions for certain procedures.
In some cases, certain insurance plans or programs may fully cover the cost of surgery, leaving the patient with no financial responsibility.
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields