Endometriosis Can Cause Infertility
Endometriosis can contribute to infertility by causing structural abnormalities, hormonal imbalances, inflammation, and the formation of adhesions that can impair fertility.
Endometriosis is characterized by the presence of tissue similar to the lining of the uterus outside of it, leading to chronic inflammation, the formation of scar tissue, and adhesions that can potentially alter the pelvic structure of a woman.
Endometriosis can lead to infertility through various mechanisms, including the formation of adhesions that can block or distort the fallopian tubes, impairing the transport of eggs and sperm; the development of endometriomas (cysts) in the ovaries, which can affect egg quality and ovulation; hormonal imbalances that disrupt the menstrual cycle and impair implantation of a fertilized egg; and the presence of chronic inflammation, which can negatively impact fertility at multiple levels.
Chances of Achieving Pregnancy with Endometriosis
- According to Counseller, V. S. (1938), “About 25 to 50% of infertile women have endometriosis, and 30 to 50% of women with endometriosis are infertile.”
- Age factor: Among women with primary infertility, half were able to have children after being diagnosed with endometriosis, and by the age of 40, 83% of all women with endometriosis had become mothers (Prescott et al., 2016).
Primary infertility refers to a situation where a couple has never been able to conceive a pregnancy after having unprotected sexual intercourse for a certain period of time (usually one year) without using any contraceptive methods.
- Women with endometriosis have a smaller likelihood of becoming pregnant each month (2-10%) compared to women without endometriosis (15-20%) (The American Society of Reproductive Medicine (ASRM), 2016).
- Egg Quality: A study conducted by Goud and colleagues in 2014 using the same method of in vitro maturation (IVM), discovered that a greater proportion of oocytes obtained from women with endometriosis had abnormal spindles compared to women undergoing assisted reproductive technology (ART) due to male factor issues (66.7% vs. 16%).
Oocytes refer to immature eggs or egg cells present in the ovaries. They are the female reproductive cells that have the potential to develop into mature eggs and be fertilized by sperm to initiate pregnancy.
Spindles are special structures that help cells divide and distribute their genetic material correctly. They act like a framework made of tiny tubes called microtubules, which help separate chromosomes during cell division. Abnormal spindles can cause problems with the division process and may lead to issues with the genetic material in the cells or embryos.
- Miscarriage and Ectopic Pregnancy: An extensive study in Scotland over a 30-year period (1981–2010) indicated that of the 5,375 pregnant women with endometriosis who participated in the study, compared to 8,280 pregnant women without endometriosis, the risk of miscarriage was 76% higher and the risk of ectopic pregnancy was three times greater in women with endometriosis (Saraswat et al, 2017).
Ectopic pregnancy is when a fertilized egg grows outside of the uterus, usually in the fallopian tube, instead of inside the uterus where a normal pregnancy occurs.
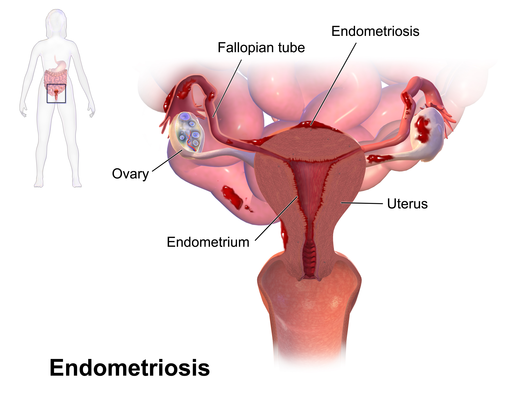
Endometriosis (Image source: Blausen Medical, 2014)
Adhesions
Adhesions formed as a result of endometriosis can contribute to infertility by affecting various reproductive structures and processes. Endometriosis-related adhesions are abnormal bands of scar tissue that develop as a response to inflammation caused by endometrial tissue outside the uterus. These adhesions can form between pelvic organs such as the ovaries, fallopian tubes, uterus, and surrounding tissues.
The presence of adhesions can lead to structural changes and functional impairments in the reproductive system, resulting in infertility. Adhesions may cause the fallopian tubes to become blocked or partially obstructed, preventing the fertilization of eggs by sperm. Additionally, adhesions can distort the normal anatomy of the pelvic organs, making it difficult for the fallopian tubes to pick up eggs released during ovulation or impairing the transport of embryos from the tubes to the uterus. This can significantly reduce the chances of conception.
Furthermore, adhesions can disrupt the natural movement and function of the fallopian tubes, affecting their ability to transport eggs and sperm. Adhesions may also hinder the implantation of a fertilized egg into the uterus, making it challenging for a pregnancy to establish and progress successfully. The severity and extent of adhesions can vary, and the impact on fertility can depend on factors such as their location, size, and the degree of obstruction or distortion they cause.
Endometriomas (Ovarian Cyst)
Endometriomas, which are cysts formed by endometriosis within the ovaries, can contribute to infertility through several mechanisms.
Firstly, the presence of endometriomas can impair ovarian function and egg quality. The cysts can disrupt the normal functioning of the ovaries, affecting the release of mature eggs during ovulation. This can result in irregular or absent ovulation, reducing the chances of fertilization.
Secondly, endometriomas can cause structural changes within the ovaries. As the cysts grow, they can distort the ovarian tissue and potentially damage the surrounding ovarian follicles, which contain the eggs. This can lead to a decreased ovarian reserve and a reduced number of viable eggs available for fertilization.
Moreover, endometriomas can create an unfavorable environment for fertilization and embryo implantation. The cysts produce substances and inflammatory factors that can affect the quality of the surrounding ovarian tissue and impair the ability of the fallopian tubes to pick up and transport eggs. Additionally, the presence of endometriomas can result in the formation of adhesions and scar tissue in the pelvis, further compromising the normal functioning of the reproductive organs.
Lastly, the surgical removal of endometriomas, while often necessary to alleviate symptoms and improve fertility, can also have an impact. The surgery itself may cause damage to healthy ovarian tissue, potentially reducing ovarian function and the number of remaining eggs.
Hormonal Imbalances
Hormonal imbalances resulting from endometriosis can contribute to infertility by disrupting the normal reproductive processes necessary for conception and pregnancy.
Endometriosis is associated with alterations in hormone levels, particularly involving estrogen and progesterone. These hormonal imbalances can disrupt the menstrual cycle, affecting ovulation, the release of mature eggs from the ovaries, and the thickening and shedding of the uterine lining.
In some cases, endometriosis can lead to anovulation, which is the absence of ovulation. Without ovulation, there are no eggs available for fertilization by sperm, significantly reducing the chances of conception. Hormonal imbalances can also cause irregular or unpredictable menstrual cycles, making it challenging to identify the fertile window for timing intercourse.
Furthermore, hormonal imbalances can impact the quality of the endometrial lining in the uterus. The endometrium undergoes changes throughout the menstrual cycle, preparing for the implantation of a fertilized egg. In endometriosis, hormonal imbalances can lead to an inadequate development of the endometrium or abnormal changes, making it difficult for an embryo to implant and establish a pregnancy.
Additionally, hormonal imbalances associated with endometriosis can contribute to the development of other reproductive issues, such as the formation of ovarian cysts (endometriomas) or the growth of endometrial tissue outside the uterus. These factors further complicate fertility by affecting ovarian function, impairing the release of mature eggs, and potentially causing adhesions that block or distort the fallopian tubes.
Addressing hormonal imbalances caused by endometriosis often involves medical interventions, such as hormonal therapy or medications that regulate the menstrual cycle. These treatments aim to restore hormonal balance, promote regular ovulation, and optimize the conditions for conception and pregnancy.
Inflammation
Inflammation resulting from endometriosis can contribute to infertility through various mechanisms that affect reproductive organs and processes.
- Disrupted Egg Quality: Chronic inflammation can impact the quality of eggs produced by the ovaries, making them less viable for fertilization and subsequent embryo development.
- Impaired Ovulation: Inflammatory factors associated with endometriosis can disrupt the normal hormonal signaling necessary for ovulation. This can lead to irregular or absent ovulation, reducing the chances of fertilization.
- Fallopian Tube Dysfunction: Inflammation can affect the functioning of the fallopian tubes, hindering their ability to pick up eggs released during ovulation, impairing the transport of sperm, and preventing the successful fertilization of eggs.
- Endometrial Abnormalities: Inflammatory processes in the pelvic region can cause structural changes and abnormalities in the endometrial lining, making it less receptive to embryo implantation.
- Increased Immune Activity: In individuals with endometriosis, the immune system may respond abnormally, leading to increased immune activity in the pelvic region. This heightened immune response can target and attack embryos or sperm, hindering successful fertilization and implantation.
- Formation of Adhesions: Inflammation can contribute to the formation of adhesions and scar tissue, leading to pelvic adhesions that can distort reproductive organs and block the fallopian tubes. This can obstruct the passage of eggs, sperm, and embryos, making conception difficult.
- Altered Hormonal Balance: Inflammatory processes can disrupt the normal hormonal balance in the body, affecting the regulation of the menstrual cycle, ovulation, and overall reproductive function.
Addressing inflammation due to endometriosis often involves a multi-faceted approach. It may include medical treatments to reduce inflammation, manage pain, and regulate the menstrual cycle. In some cases, surgical interventions, such as laparoscopy, may be necessary to remove endometrial implants, adhesions, or cysts that contribute to inflammation. Fertility treatments, such as assisted reproductive techniques like IVF, may also be recommended to bypass the effects of inflammation and improve the chances of achieving pregnancy.
Endometrial Abnormalities
Endometrial abnormalities can contribute to infertility by affecting the implantation of embryos and the development of a healthy pregnancy. Here are four ways in which endometrial abnormalities can impact fertility:
- Impaired Implantation: The endometrial lining plays a crucial role in the successful implantation of a fertilized embryo. Abnormalities in the endometrium, such as thinning, insufficient development, or structural irregularities, can make it difficult for embryos to properly attach and implant into the uterine wall.
- Insufficient Secretory Function: The endometrium undergoes changes during the menstrual cycle to support the growth and development of an implanted embryo. In some cases of endometrial abnormalities, the endometrium may not adequately develop the necessary secretory function, compromising the nourishment and support required for embryo implantation and early pregnancy.
- Abnormal Blood Flow: Endometrial abnormalities can affect the blood flow within the uterine lining, leading to inadequate circulation or reduced oxygen and nutrient supply to the developing embryo. This can hinder the establishment and maintenance of a healthy pregnancy.
- Structural Defects: Structural abnormalities in the uterus, such as uterine septum or polyps within the endometrium, can interfere with embryo implantation and increase the risk of early pregnancy loss.
Addressing endometrial abnormalities often involves a thorough evaluation of the uterus and the endometrium. Depending on the specific abnormality, treatments may include hormonal therapies to improve endometrial development, surgical interventions to correct structural defects, or assisted reproductive techniques like embryo transfer.
Decreased Ovarian Reserve
Decreased ovarian reserve resulting from endometriosis can significantly impact fertility by reducing the quantity and quality of eggs available for fertilization. Here’s how this process can affect infertility:
- Diminished Egg Quantity: Endometriosis can lead to a reduction in the number of eggs within the ovaries. The presence of endometriotic cysts, also known as endometriomas, can damage ovarian tissue and deplete the pool of viable eggs. As a result, there may be fewer eggs available for ovulation and fertilization.
- Impaired Egg Quality: Endometriosis can affect the quality of eggs within the ovaries. The inflammatory environment associated with endometriosis can lead to oxidative stress and DNA damage in the eggs, resulting in lower egg quality. Reduced egg quality can hinder successful fertilization and increase the risk of chromosomal abnormalities, leading to a higher chance of miscarriage or failed implantation.
- Altered Ovarian Function: Endometriosis can disrupt normal ovarian function. The presence of endometriomas or adhesions can interfere with the release of eggs during ovulation or block the fallopian tubes, preventing the eggs from reaching the site of fertilization.
- Surgical Interventions: Surgical procedures to treat endometriosis, such as cyst removal or ovarian surgery, can inadvertently damage ovarian tissue and decrease ovarian reserve. While these procedures may be necessary to alleviate symptoms or improve fertility potential, they can further diminish the number of available eggs.
- Early Ovarian Aging: Endometriosis is associated with an accelerated decline in ovarian reserve, leading to premature ovarian aging. This means that individuals with endometriosis may experience a decline in ovarian function and egg supply at a younger age compared to those without the condition, potentially impacting fertility at an earlier stage of life.
Understanding the impact of decreased ovarian reserve is crucial for managing fertility in individuals with endometriosis. Fertility preservation techniques, such as egg freezing, may be considered for those who want to preserve their eggs before their ovarian reserve further declines.
In cases where natural conception is challenging, assisted reproductive technologies like in vitro fertilization (IVF) or the use of donor eggs may be recommended to improve the chances of successful pregnancy.
What is Silent Endometriosis?
Silent endometriosis, also known as asymptomatic endometriosis, refers to a condition where a person has endometriosis, but they do not experience any noticeable symptoms.
Silent endometriosis can be challenging to diagnose because the absence of symptoms may lead to a delay in seeking medical attention or a misdiagnosis. It is often discovered incidentally during diagnostic procedures for other conditions or during infertility evaluations.
When undergoing multiple IVF cycles, if silent endometriosis is present, it can affect the success rates of the treatment. Endometriosis can cause inflammation, hormonal imbalances, and the formation of scar tissue, all of which can impact the implantation of the embryo and the overall outcome of the IVF cycle.
It’s important to note that even if a person with silent endometriosis does not experience symptoms, the condition can still have long-term consequences. Endometriosis can progress over time and potentially lead to fertility problems or the formation of scar tissue and adhesions in the pelvic area.
Endometriosis Staging System
A classification system exists to assess the severity or stage of endometriosis:
- Stage I endometriosis (minimal disease) is characterized by a few small endometriotic implants without any observed scar tissue.
- Stage II endometriosis (mild disease) involves more implants of endometriosis, but the affected area is less than 2 inches in the abdomen, and no scar tissue is present.
- Stage III endometriosis (moderate disease) manifests as a substantial presence of endometriosis throughout the abdomen, potentially extending deeply and forming pockets of endometriotic fluid (endometriomas) in the ovaries. Scar tissue may be present around the fallopian tubes or ovaries.
- Stage IV endometriosis signifies a significant number of endometriotic implants, potentially including large cysts in the ovaries (endometriomas), extensive scar tissue between the uterus and the rectum (lower part of the intestines), and around the ovaries or fallopian tubes.
Surgical Treatment of Endometriosis and Fertility
Women diagnosed with Stage I and II endometriosis may achieve pregnancy naturally; however, studies suggest that infertility patients who undergo laparoscopy are more likely to have endometriosis compared to women who conceive without difficulty. Surgical removal of Stage I or II endometriosis may potentially enhance pregnancy rates, although conflicting data exists on its efficacy.
Generally, in younger women (under 35 years old), it is reasonable to consider the removal of visible endometriosis to assess natural conception. For women aged 35 and above, alternative fertility treatments are typically recommended instead of laparoscopy. In cases of Stage III or IV endometriosis, surgical intervention to eliminate scar tissue or large endometriotic cysts can lead to improved pregnancy rates. If pregnancy does not occur within six months following surgical treatment, alternative fertility treatments should be discussed.
Unfortunately, some women with endometriosis may experience recurrent cysts. Repeated removal of cysts can result in diminished ovarian reserve and increase the challenges of achieving pregnancy.
Surgical Methods for Endometriosis Treatment
There are several surgical methods used for the treatment of endometriosis to improve fertility. These procedures aim to remove or reduce endometriotic lesions, adhesions, and other abnormalities that may be affecting reproductive function.
Here are some common surgical methods used for endometriosis treatment to improve fertility:
Laparoscopy
Laparoscopy is a surgical procedure commonly used to diagnose and treat endometriosis. While it can help alleviate symptoms and improve fertility outcomes in some cases, it is important to note that laparoscopy may not guarantee a cure for infertility caused by endometriosis. Here’s a closer look at how laparoscopy can be used in the context of infertility:
- Diagnosis: Laparoscopy is often performed to visually confirm the presence and extent of endometriosis. During the procedure, the surgeon uses a laparoscope (a thin, lighted instrument) to examine the pelvic organs and identify endometrial implants, adhesions, and cysts. Confirming the diagnosis of endometriosis is a crucial step in managing infertility associated with the condition.
- Surgical Removal: Laparoscopy allows for the surgical removal or ablation of endometrial implants, scar tissue, and ovarian cysts (endometriomas). Removing these growths and adhesions can help improve fertility outcomes by restoring normal pelvic anatomy and reducing the inflammatory environment associated with endometriosis.
- Enhancing Egg Quality: In cases where endometriomas are present, laparoscopy can be used to drain or remove these cysts. By reducing the presence of endometriomas, the surgery may help improve egg quality and ovarian function.
- Restoring Fallopian Tube Function: Laparoscopy can address fallopian tube dysfunction caused by endometriosis, such as removing adhesions or opening blocked tubes. Restoring normal fallopian tube function improves the chances of eggs being picked up, transported, and fertilized.
- Adjunct to Fertility Treatments: Laparoscopy is often used in conjunction with other fertility treatments, such as in vitro fertilization (IVF). By surgically addressing endometriosis, laparoscopy can improve the success rates of fertility treatments by creating a more favorable environment for embryo implantation.
It’s important to note that the effectiveness of laparoscopy in improving fertility outcomes varies depending on factors such as the severity of endometriosis, age, and individual circumstances.
We Accept Most Major Insurance Plans. Surgeries are typically covered by health insurance. However, the extent of coverage can vary depending on the specific insurance plan and policy. Some insurance plans may cover a broad range of surgical procedures, including both elective and necessary surgeries, while others may have limitations or exclusions for certain procedures.
In some cases, certain insurance plans or programs may fully cover the cost of surgery, leaving the patient with no financial responsibility.
It is recommended to request an appointment with New York Gynecology Endometriosis (NYGE) who can evaluate the specific situation and provide personalized guidance on the most appropriate treatment options for infertility related to endometriosis.
Excision Surgery
Excision surgery is a highly effective surgical method for treating endometriosis and improving fertility outcomes. This surgical technique involves the complete removal of endometriotic lesions, including deeply infiltrating endometriosis (DIE) and superficial implants. Here’s how excision surgery can help improve fertility:
- Removal of Endometriotic Lesions: Excision surgery aims to completely excise endometriotic lesions from affected areas, such as the ovaries, fallopian tubes, uterus, and pelvic cavity. By removing these abnormal growths, the surgery helps restore the normal anatomy and function of reproductive organs.
- Preservation of Healthy Tissue: During excision surgery, the surgeon carefully identifies and removes endometriotic lesions while preserving healthy tissue. This approach minimizes damage to the surrounding structures and reduces the risk of recurrence.
- Reduction of Inflammation: Endometriotic lesions are associated with chronic inflammation, which can negatively impact fertility. By removing the lesions, excision surgery helps reduce the inflammatory response in the pelvic cavity, creating a more favorable environment for fertility.
- Restoration of Ovarian Function: Endometriotic lesions, particularly endometriomas (cysts in the ovaries), can affect ovarian function and diminish fertility. Excision surgery, specifically ovarian cystectomy, involves removing these cysts while preserving healthy ovarian tissue. This helps improve ovarian function and enhances the quality of eggs available for fertilization.
- Reduction of Pelvic Adhesions: Endometriosis can cause adhesions (scar tissue) to form in the pelvic cavity, which may lead to infertility by blocking the fallopian tubes or interfering with the normal movement of eggs and sperm. Excision surgery addresses these adhesions, restoring the patency and function of the fallopian tubes and improving the chances of natural conception.
- Enhanced Response to Fertility Treatments: By eliminating endometriotic lesions and reducing inflammation, excision surgery can enhance the response to fertility treatments, such as in vitro fertilization (IVF). Improved reproductive organ function and a healthier pelvic environment increase the chances of successful embryo implantation and pregnancy.
Robotic Assisted Surgery
Robotic-assisted surgery is a minimally invasive surgical technique that can be used to treat infertility caused by endometriosis. Here’s how robotic-assisted surgery can help in the treatment of endometriosis-related infertility:
- Precise and Magnified Visualization: Robotic-assisted surgery utilizes a high-definition camera and a three-dimensional view, providing the surgeon with enhanced visualization of the pelvic structures. This allows for precise identification and removal of endometriotic lesions while minimizing damage to healthy tissue.
- Improved Surgical Precision: The robotic surgical system provides the surgeon with precise control over surgical instruments, which can maneuver in a more flexible manner than traditional laparoscopic instruments. This enhanced dexterity allows for delicate manipulation of tissues and improved surgical precision, particularly when dealing with complex endometriotic lesions or areas requiring meticulous dissection.
- Reduced Trauma and Scarring: Robotic-assisted surgery uses small incisions, similar to traditional laparoscopy, resulting in less trauma to the body compared to open surgery. The smaller incisions minimize scarring, reduce post-operative pain, and contribute to faster recovery times.
- Enhanced Reach and Accessibility: The robotic surgical system’s flexible instruments and articulating arms can access hard-to-reach areas, such as deep-seated endometriotic lesions or areas near delicate structures like the fallopian tubes or ovaries. This improved access allows for thorough excision of endometriotic lesions, including deep infiltrating endometriosis (DIE), which may be crucial for restoring fertility.
- Reduced Blood Loss: The precise movements and cauterization capabilities of the robotic instruments can minimize blood loss during surgery, promoting a safer surgical environment and reducing the need for blood transfusions.
- Shorter Hospital Stay: Robotic-assisted surgery is minimally invasive, which often translates into a shorter hospital stay compared to open surgery. Patients may experience a quicker recovery and return to their daily activities sooner.
It’s important to note that the suitability of robotic-assisted surgery for treating infertility due to endometriosis depends on the individual case and the surgeon’s expertise. A thorough evaluation by a skilled endometriosis surgeon such as Dr Pankaj Singhal or other fertility specialist is necessary to determine the most appropriate surgical approach for addressing endometriosis-related infertility.
Ovarian Cystectomy
Endometriomas, which are cysts formed from endometriotic tissue in the ovaries, can interfere with fertility. Ovarian cystectomy involves the removal of these cysts while preserving the ovarian tissue. This procedure helps improve ovarian function and egg quality.
Uterine Surgery
In cases where endometriosis affects the uterus, surgical interventions like hysteroscopy or myomectomy may be performed. Hysteroscopy involves the removal of endometrial polyps or submucosal fibroids that may be interfering with implantation or causing abnormal bleeding. Myomectomy addresses the removal of uterine fibroids, which can also impact fertility.
Salpingectomy or Tubal Surgery
If endometriosis has caused significant damage to the fallopian tubes, such as blockages or severe adhesions, surgical removal of the affected portion (salpingectomy) or repair of the tubes (tubal surgery) may be considered. These procedures aim to restore normal tubal function and improve the chances of natural conception.
References
Goud, P. T., Goud, A. P., Joshi, N., Puscheck, E., Diamond, M. P., & Abu-Soud, H. M. (2014). Dynamics of nitric oxide, altered follicular microenvironment, and oocyte quality in women with endometriosis. Fertility and sterility, 102(1), 151–159.e5. https://doi.org/10.1016/j.fertnstert.2014.03.053
Prescott, J., Farland, L. V., Tobias, D. K., Gaskins, A. J., Spiegelman, D., Chavarro, J. E., Rich-Edwards, J. W., Barbieri, R. L., & Missmer, S. A. (2016). A prospective cohort study of endometriosis and subsequent risk of infertility. Human reproduction (Oxford, England), 31(7), 1475–1482. https://doi.org/10.1093/humrep/dew085
Practice Committee of the American Society for Reproductive Medicine (2004). Endometriosis and infertility. Fertility and sterility, 81(5), 1441–1446. https://doi.org/10.1016/j.fertnstert.2004.01.019
Saraswat, L., Ayansina, D. T., Cooper, K. G., Bhattacharya, S., Miligkos, D., Horne, A. W., & Bhattacharya, S. (2017). Pregnancy outcomes in women with endometriosis: a national record linkage study. BJOG : an international journal of obstetrics and gynaecology, 124(3), 444–452. https://doi.org/10.1111/1471-0528.13920
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries. Learn more >

We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage.
Surgeries are typically covered by health insurance. However, the extent of coverage can vary depending on the specific insurance plan and policy. Some insurance plans may cover a broad range of surgical procedures, including both elective and necessary surgeries, while others may have limitations or exclusions for certain procedures.
In some cases, certain insurance plans or programs may fully cover the cost of surgery, leaving the patient with no financial responsibility.
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields