Endometrioma and Fertility
Endometrioma, a cystic lesion of the ovaries associated with endometriosis, may affect fertility, but the impact on reproductive health and the optimal management strategy require further investigation.
Endometrioma is a type of cystic lesion that forms on the ovaries. It arises from the glands and tissue similar to the lining of the uterus called endometrium. About 17-44% of patients with endometriosis have these cysts (Muzzi et al., 2017).
During infertility screening, it is commonly observed that 30-50% of females diagnosed with endometriosis have endometriomas, indicating a correlation between these cystic lesions and fertility problems (Macer et al., 2012).
Existing evidence suggests that endometrioma may affect a woman’s reproductive health by impairing her ovarian reserve. This can happen due to the cysts taking up space in the ovaries or causing a local reaction, or both. To prevent further damage to the ovaries, surgical removal of endometrioma has often been recommended. However, recent focus has shifted towards understanding the potential negative impact of this surgery on the ovarian reserve.
The controversy lies in whether or not surgical removal of endometrioma can improve a woman’s chances of getting pregnant, especially for young females who are planning to conceive. A review of the effects of endometrioma and its removal in females undergoing assisted reproductive technology (ART) suggests that prior surgery for endometrioma may not lead to better fertility outcomes. In fact, it may result in a decreased number of eggs retrieved in affected females.
Therefore, further studies are needed to determine the best approach for managing infertility in women with endometriomas. The optimal management strategy should consider the potential impact on ovarian reserve and assist in improving fertility outcomes in this specific context.
Ovarian Reserves and Hormones
The number of eggs a woman has is determined before birth, with approximately six to seven million eggs present midway through her mother’s pregnancy. After birth, this number decreases to about a million, and by puberty, it further reduces to 300,000 to 500,000 eggs. As menopause approaches, the number dwindles to around 1,000 eggs. Fertility decline becomes more significant in the mid-30s due to diminishing ovarian reserve.
To assess ovarian reserve, various tests are employed, often referred to using acronyms such as FSH (follicle-stimulating hormone), AMH (anti-Mullerian hormone), and AFC (antral follicle count).
Follicle-Stimulating Hormone (FSH): FSH is produced by the pituitary gland and is responsible for stimulating the growth and development of follicles in the ovaries. It plays a crucial role in the maturation of eggs and the overall reproductive process.
Luteinizing Hormone (LH): LH is also produced by the pituitary gland and works in conjunction with FSH. It triggers ovulation, which is the release of a mature egg from the ovary. LH surge is essential for successful conception.
- Antral Follicle Count (AFC): Antral follicle count (AFC) is a method used to assess ovarian reserve by counting the number of small fluid-filled sacs, called antral follicles, present in the ovaries. A higher AFC suggests a larger pool of immature eggs and potentially higher fertility potential, while a lower AFC may indicate diminished ovarian reserve.
Estrogen: Estrogen is primarily produced by the ovaries and plays a vital role in regulating the menstrual cycle. It helps stimulate the growth of the uterine lining (endometrium) and supports the development of a healthy environment for implantation of a fertilized egg.
Progesterone: Progesterone is produced by the ovaries after ovulation and is crucial for preparing the uterus for pregnancy. It helps thicken the uterine lining and promotes the implantation and maintenance of a fertilized egg.
Anti-Mullerian Hormone (AMH): AMH is produced by the follicles in the ovaries and serves as an indicator of ovarian reserve. It provides an estimate of the number of eggs remaining in a woman’s ovaries and is used as a predictor of fertility potential.
Endometrioma and Hormonal Impact
In the context of endometrioma, the presence and development of these hormones can be affected. Endometrioma is a cystic lesion of the ovaries that originates from endometrial tissue, which is responsive to hormonal changes.
- FSH and LH: Endometrioma can disrupt the normal hormonal feedback loop involving FSH and LH. The presence of endometrioma can lead to altered FSH and LH levels, affecting follicle development, ovulation, and the release of mature eggs.
- Antral Follicle Count: The presence of endometriomas can affect the accuracy of Antral Follicle Count (AFC) as a measure of ovarian reserve. Endometriomas can distort the ovarian architecture and potentially reduce the number of visible antral follicles during ultrasound examination. This can lead to an underestimation of the AFC and may not reflect the true ovarian reserve in individuals with endometriomas.
- Estrogen: Endometrioma can contribute to increased production of estrogen within the affected ovarian tissue. This may result in higher estrogen levels circulating in the body, which can promote the growth and persistence of endometrioma as well as exacerbate the symptoms associated with endometriosis.
- Progesterone: Endometrioma can interfere with the normal production and action of progesterone. This may disrupt the balance between estrogen and progesterone, leading to an imbalance that can negatively impact the development and maintenance of the uterine lining, potentially affecting fertility and implantation.
- Anti-Mullerian Hormone (AMH): Endometrioma can have an impact on ovarian reserve and consequently affect AMH levels. The presence of endometrioma may reduce the number of healthy follicles available, potentially leading to a decrease in AMH levels.
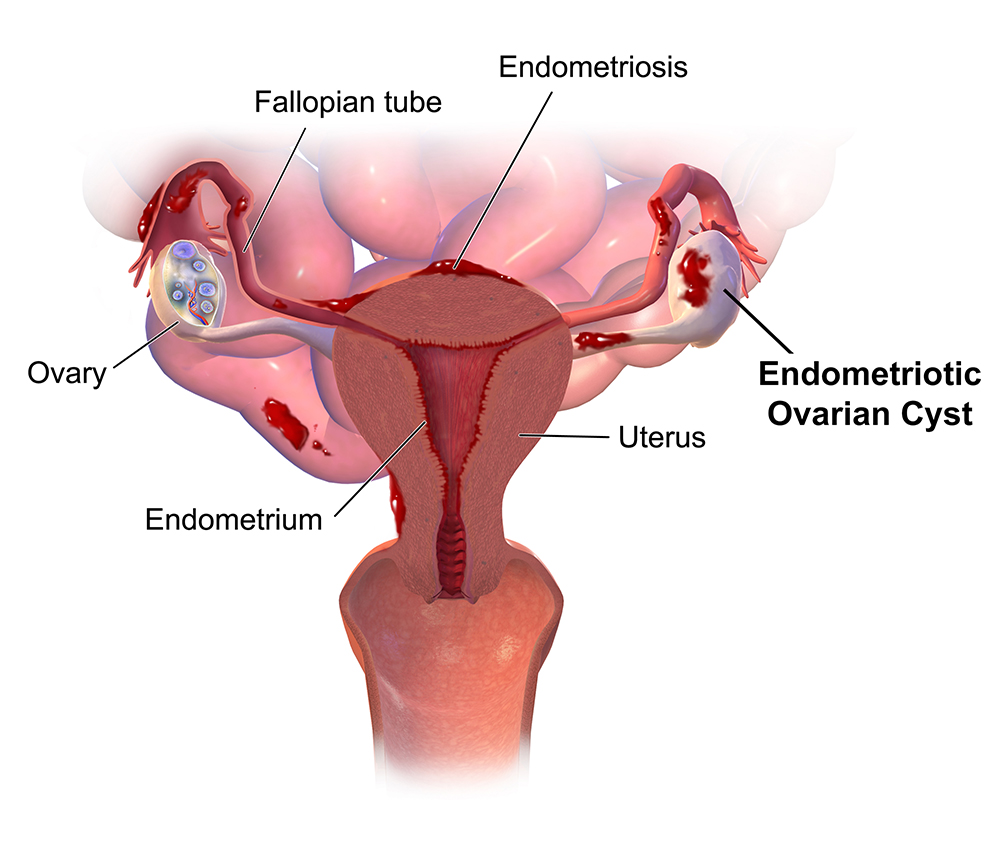
Endometriosis (Image source: Blausen Medical, 2014)
IVF as a Treatment for Infertility in Cases of Endometrioma
In vitro fertilization (IVF) is a common treatment option for infertility associated with endometrioma. IVF involves stimulating the ovaries to produce multiple eggs, retrieving the mature eggs, fertilizing them with sperm in a laboratory setting, and then transferring the resulting embryos into the uterus.
For women with endometrioma, IVF can be particularly beneficial because it bypasses the potential barriers to conception posed by the presence of the cystic lesions. By directly retrieving eggs from the ovaries and fertilizing them outside the body, IVF circumvents any impairment caused by endometrioma in the natural reproductive process.
However, it is important to note that the decision to pursue IVF for endometrioma-associated infertility should be made on an individual basis. Factors such as the severity of endometriosis, the size and location of the endometrioma, and the overall fertility status of the individual should be considered.
Additionally, it is recommended to consult with a fertility specialist who can assess the specific situation and provide personalized guidance on the most suitable treatment options, which may include IVF or other interventions, based on the unique needs and goals of the individual.
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries. Learn more >

We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage.
Surgeries are typically covered by health insurance. However, the extent of coverage can vary depending on the specific insurance plan and policy. Some insurance plans may cover a broad range of surgical procedures, including both elective and necessary surgeries, while others may have limitations or exclusions for certain procedures.
In some cases, certain insurance plans or programs may fully cover the cost of surgery, leaving the patient with no financial responsibility.
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields