Peritoneal Endometriosis
Peritoneal endometriosis refers to the presence and growth of endometrial tissue outside the uterus, specifically within the peritoneum, causing pain and potential complications.
The American Society of Reproductive Medicine (ASRM) defines peritoneal endometriosis as the presence of endometrial tissue outside the uterus, specifically within the peritoneal cavity. This tissue can implant and grow on various structures within the peritoneum, including the pelvic organs, abdominal wall, and diaphragm.
Peritoneal endometriosis can lead to the formation of implants, adhesions, and cysts, causing symptoms such as pelvic pain, infertility, and menstrual irregularities. The ASRM recognizes peritoneal endometriosis as a common and significant condition affecting reproductive-aged women. Treatment options for peritoneal endometriosis may include pain management, hormonal therapies, or surgical interventions, with the goal of alleviating symptoms and improving fertility when desired.
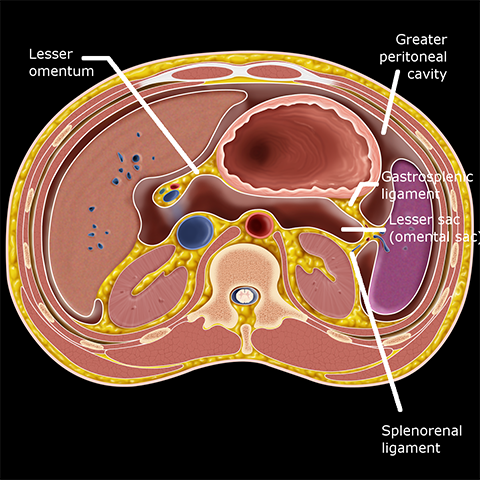
Peritoneal Cavity (Image source: Stanford)
Subtype of Peritoneal Endometriosis
There are different subtypes of peritoneal endometriosis based on the location and characteristics of the endometrial implants within the peritoneum. Some of the common subtypes include:
- Superficial peritoneal endometriosis: This subtype involves small, superficial implants or lesions on the surface of the peritoneum.
- Deep infiltrating peritoneal endometriosis (DIPE): In this subtype, endometrial tissue infiltrates deeply into the peritoneal tissue, extending beyond the surface. It can involve structures such as the bowel, bladder, ureters, and pelvic sidewalls.
- Ovarian endometriosis: This subtype specifically refers to the presence of endometriosis on or within the ovaries, forming cysts called endometriomas.
- Rectovaginal endometriosis: This subtype involves the presence of endometrial implants between the rectum and the vagina, causing pain, inflammation, and potential complications.
These subtypes can coexist or occur individually, and the severity and symptoms can vary from person to person. Proper diagnosis and classification of the subtype are important for effective management and treatment planning.
Why is Peritoneal Endometriosis So Unique?
Peritoneal endometriosis is a unique condition because it involves the abnormal growth of endometrial tissue outside the uterus, specifically on the peritoneum, which is the tissue lining the abdominal cavity. Here are a few reasons why peritoneal endometriosis is considered unique:
Location: Peritoneal endometriosis occurs in the peritoneal cavity, which is an uncommon site for endometrial tissue growth. Normally, endometrial tissue is found lining the inner wall of the uterus. When it grows outside the uterus, it can implant on various structures within the peritoneal cavity, such as the ovaries, fallopian tubes, bladder, intestines, and other abdominal organs.
Mechanism of spread: The exact cause of endometriosis is not fully understood, but there are several theories. One theory is retrograde menstruation, where menstrual blood containing endometrial cells flows backward through the fallopian tubes into the pelvic cavity. However, the spread of endometriosis to the peritoneal cavity involves additional factors that allow the endometrial cells to attach, invade, and grow on the peritoneal surface.
Diverse symptoms: Peritoneal endometriosis can present with a wide range of symptoms, including pelvic pain, painful periods, pain during intercourse, irregular bleeding, infertility, and gastrointestinal symptoms such as bloating, constipation, or diarrhea. The symptoms can vary in intensity and may not always correlate with the severity of the condition.
Diagnostic challenges: Diagnosing peritoneal endometriosis can be challenging because its symptoms overlap with other conditions such as pelvic inflammatory disease, irritable bowel syndrome, and ovarian cysts. Additionally, the gold standard for definitive diagnosis is through laparoscopic surgery with tissue biopsy, which is an invasive procedure.
Impact on fertility: Peritoneal endometriosis can affect fertility by causing inflammation, scarring, and adhesions that can impair the function of the ovaries, fallopian tubes, and uterus. The abnormal tissue growth and associated structural changes can disrupt the normal processes of ovulation, fertilization, and implantation, making it more difficult for a woman to conceive.
Recurrence and persistence: Peritoneal endometriosis can be a chronic condition with a tendency to recur even after surgical removal or medical treatment. This is because some endometrial cells may remain or regrow after treatment, and the hormonal fluctuations during the menstrual cycle can stimulate their growth.
It’s important to note that while peritoneal endometriosis is unique in its characteristics, there are other forms of endometriosis, such as ovarian endometriosis and deep infiltrating endometriosis, which also have their own distinctive features.
Diagnosis of Peritoneal Endometriosis
The diagnosis of peritoneal endometriosis typically involves a combination of medical history evaluation, physical examination, imaging tests, and, in many cases, a definitive confirmation through surgical intervention. Here are the common steps involved in diagnosing peritoneal endometriosis:
Medical history and symptom evaluation: The doctor will review your medical history and ask about your symptoms, such as pelvic pain, painful periods, infertility, or gastrointestinal issues. Providing detailed information about the nature, severity, and timing of your symptoms can assist in the diagnostic process.
Physical examination: A pelvic examination may be performed to check for any abnormalities, tenderness, or masses in the pelvic region. However, it’s important to note that physical examination alone cannot provide a definitive diagnosis of peritoneal endometriosis.
Imaging tests: Imaging studies such as transvaginal ultrasound (TVUS) or pelvic ultrasound may be conducted to visualize the pelvic organs and look for any signs of endometriosis, such as ovarian cysts (endometriomas) or deep infiltrating lesions. However, these imaging tests may not always provide conclusive evidence of peritoneal endometriosis.
Laparoscopy: Laparoscopic surgery is considered the gold standard for the diagnosis of peritoneal endometriosis. It is a minimally invasive procedure where a thin, lighted tube with a camera (laparoscope) is inserted through small incisions in the abdomen. This allows the surgeon to directly visualize and examine the pelvic organs and peritoneum for the presence of endometrial implants, adhesions, and other characteristic signs of endometriosis. Tissue samples (biopsies) may also be taken during laparoscopy for histological examination to confirm the presence of endometrial tissue.
It’s important to consult with a healthcare professional who specializes in endometriosis diagnosis and treatment for an accurate evaluation and management of peritoneal endometriosis. Each case is unique, and the diagnostic process may vary depending on individual circumstances.
Peritoneal Endometriosis and the Immune System
Peritoneal endometriosis involves the presence of endometrial tissue outside the uterus, specifically within the peritoneal cavity. The immune system plays a crucial role in the development and progression of endometriosis, including peritoneal endometriosis. Here’s how the immune system interacts with peritoneal endometriosis:
Inflammatory response: The presence of endometrial tissue outside the uterus triggers an inflammatory response within the peritoneal cavity. Immune cells, such as macrophages and T cells, are recruited to the affected areas and release various inflammatory molecules and cytokines. This inflammation contributes to the symptoms associated with peritoneal endometriosis, such as pelvic pain and tissue damage.
Immune cell dysfunction: In women with peritoneal endometriosis, there is evidence of altered immune cell function. Some studies have shown that immune cells in the peritoneal fluid of affected individuals exhibit impaired ability to recognize and eliminate endometrial cells, leading to their survival and growth outside the uterus.
Immune tolerance: Endometriosis is characterized by the ability of endometrial cells to evade immune surveillance and establish themselves in ectopic locations. The immune system may exhibit a certain degree of tolerance towards these misplaced endometrial cells, failing to mount a robust immune response to eliminate them. This immune tolerance allows the survival and growth of endometrial implants within the peritoneal cavity.
Inflammatory mediators: The immune cells and endometrial tissue in the peritoneal cavity produce various inflammatory mediators, such as prostaglandins, cytokines, and growth factors. These molecules contribute to the development and progression of peritoneal endometriosis by promoting tissue invasion, angiogenesis (formation of new blood vessels), and the formation of adhesions between organs.
Hormonal influence: Hormones, particularly estrogen, have a significant impact on the immune response and the growth of endometriotic tissue. Estrogen can modulate immune cell function and promote the survival and proliferation of endometrial cells. It is believed that hormonal imbalances and increased estrogen levels contribute to the development and maintenance of peritoneal endometriosis.
Understanding the complex interplay between peritoneal endometriosis and the immune system is crucial for developing targeted treatment strategies. Research in this area aims to identify immune-based therapies that can modulate the immune response and improve outcomes for individuals with peritoneal endometriosis.
Surgical Treatment for Peritoneal endometriosis
Surgical treatment is often an important approach for managing peritoneal endometriosis, particularly when the symptoms are severe or when fertility preservation is a concern. The primary goal of surgical treatment is to remove or ablate the endometrial implants, alleviate symptoms, and restore normal anatomical structures within the peritoneal cavity. Here are some common surgical options for peritoneal endometriosis:
Laparoscopic Excision
Laparoscopic surgery, also known as minimally invasive or keyhole surgery, is the preferred approach for treating peritoneal endometriosis. During the procedure, small incisions are made in the abdomen, and a laparoscope (a thin, lighted tube with a camera) is inserted to visualize the pelvic organs and the peritoneal cavity. Surgical instruments are used to excise or remove the endometrial implants, adhesions, and any other abnormal tissue. This technique allows for a precise and targeted removal of the endometriotic lesions while minimizing trauma to surrounding tissues.
On average, the cost of laparoscopic excision for endometriosis can range from approximately $7,000 to $15,000 or more.
To obtain an accurate cost estimate, it is advisable to arrange an appointment with New York Gynecology Endometriosis (NYGE).
Laser Ablation
Laser ablation is a technique that uses laser energy to destroy or vaporize the endometrial implants. It is performed during laparoscopic surgery and can be effective for superficial lesions or areas that are difficult to excise. The laser energy is applied to the lesions, effectively destroying the abnormal tissue.
Deep Infiltrating Endometriosis (DIE) Surgery
In cases where peritoneal endometriosis involves deep infiltration into surrounding tissues or organs, a more extensive surgical procedure may be required. This type of surgery aims to remove the deeply infiltrating endometrial implants and restore the affected organs’ normal anatomy and function. It may involve excision, resection, or reconstruction of the affected organs, such as the bowel, bladder, or ureters. DIE surgery is often performed by experienced specialists in endometriosis and may require collaboration with other surgical specialties.
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries.

We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage.
Surgeries are typically covered by health insurance. However, the extent of coverage can vary depending on the specific insurance plan and policy. Some insurance plans may cover a broad range of surgical procedures, including both elective and necessary surgeries, while others may have limitations or exclusions for certain procedures.
In some cases, certain insurance plans or programs may fully cover the cost of surgery, leaving the patient with no financial responsibility.
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields