Uterine Fibroids
Fibroids, also known as uterine fibroids or leiomyomas, are benign (non-cancerous) growths that occur in the uterus.
Fibroids are the most common type of tumor with estimates suggesting that up to 70-80% of women may develop fibroids by the age of 50. However, not all fibroids cause symptoms, and many women may have fibroids without even knowing it.
Fibroids can vary in size, shape, and location within the uterus. They can be as small as a seed or as large as a grapefruit, and they can be found in different parts of the uterus, such as inside the uterus (submucosal), outside the uterus (subserosal), or in the wall of the uterus (intramural).
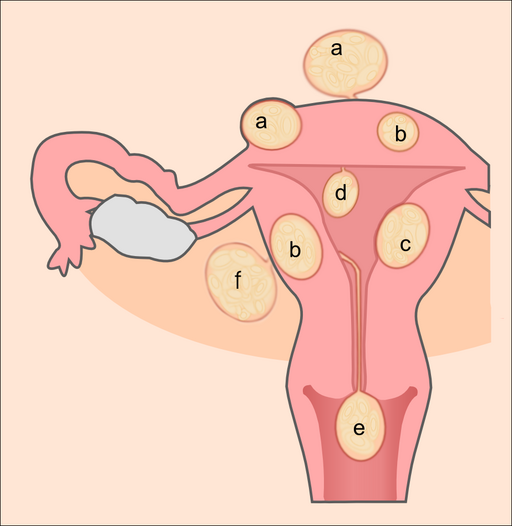
(Hic et nunc, 2012). Creative Commons license.
Classification of Uterine Fibroids
(a) subserosal fibroids
(b) intramural fibroids
(c) submucosal fibroid
(d) pedunculated submucosal fibroid
(e) fibroid in statu nascendi
(f) intraligamental fibroid
Classification of Uterine Fibroids
The three main types of fibroids based on location are submucosal fibroids, intramural fibroids, and subserosal fibroids. In addition to these three main types, there are also other less common types, such as pedunculated fibroids, fibroid in statu nascendi, and intraligamental fibroid.
(a) Subserosal Fibroids
Subserosal fibroids are a type of uterine fibroid that grow on the outer surface of the uterus, known as the serosa. They can protrude outward and may cause symptoms such as pelvic pain, pressure, and an enlarged abdomen. Here are some key characteristics of subserosal fibroids:
- Location: Subserosal fibroids are located on the outer surface of the uterus, which is covered by a layer of tissue called the serosa. They may grow as single nodules or as multiple fibroids.
- Size: Subserosal fibroids can vary in size, ranging from small fibroids that are not visible to the naked eye, to large fibroids that can cause a noticeable bulge or protrusion in the abdomen.
- Symptoms: Subserosal fibroids may cause symptoms such as pelvic pain, pressure, discomfort, or a feeling of fullness in the abdomen. They may also cause back pain, urinary frequency or urgency, and constipation if they press on nearby organs.
- Impact on fertility: Subserosal fibroids are less likely to affect fertility compared to submucosal fibroids, as they typically do not protrude into the uterine cavity. However, in some cases, large subserosal fibroids or fibroid clusters may affect fertility by causing distortion or compression of the fallopian tubes or interfering with implantation.
(b) Intramural Fibroids
Intramural fibroids are a type of uterine fibroid that grow within the muscular wall of the uterus. They are the most common type of fibroids and can cause a range of symptoms. Here are some key characteristics of intramural fibroids:
- Location: Intramural fibroids are located within the muscular layer of the uterus, known as the myometrium. They can grow as single nodules or as multiple fibroids.
- Size: Intramural fibroids can vary in size, ranging from small fibroids that are not visible to the naked eye, to large fibroids that can cause an enlargement of the uterus.
- Symptoms: Intramural fibroids may cause symptoms such as pelvic pain, pressure, heavy menstrual bleeding, prolonged menstrual periods, and an enlarged uterus. They can also cause symptoms related to compression of nearby organs, such as urinary frequency or urgency, constipation, or lower back pain.
- Impact on fertility: Intramural fibroids can sometimes affect fertility, depending on their size, location, and number. Large intramural fibroids or fibroid clusters may distort the shape of the uterus or interfere with the fallopian tubes, which can impact fertility or increase the risk of miscarriage. However, not all intramural fibroids affect fertility, and the impact on fertility varies from case to case.
(c) Submucosal Fibroids
Submucosal fibroids are a type of uterine fibroid that grow just underneath the inner lining of the uterus, known as the endometrium. They can protrude into the uterine cavity and may cause a variety of symptoms. Here are some key characteristics of submucosal fibroids:
- Location: Submucosal fibroids are located just underneath the inner lining of the uterus, and they can protrude into the uterine cavity. They are the least common type of fibroids but can cause significant symptoms.
- Size: Submucosal fibroids can vary in size, ranging from small fibroids that are not visible to the naked eye, to larger fibroids that can distort the shape of the uterus and occupy a significant portion of the uterine cavity.
- Symptoms: Submucosal fibroids are more likely to cause symptoms compared to other types of fibroids. They may cause heavy menstrual bleeding, prolonged menstrual periods, irregular bleeding, pelvic pain, pressure, and discomfort. They can also cause symptoms related to compression of the endometrium, such as infertility, recurrent miscarriages, or difficulty getting pregnant.
- Impact on fertility: Submucosal fibroids are more likely to affect fertility compared to other types of fibroids, as they can distort the shape of the uterine cavity and interfere with implantation. They may also cause recurrent miscarriages or difficulty getting pregnant.
(d) Pedunculated Submucosal Fibroids
A pedunculated submucosal fibroid is a type of benign (non-cancerous) tumor that grows in the uterus. It is characterized by a fibroid that is attached to the inner lining of the uterus, called the endometrium, by a stalk or peduncle, which allows it to protrude into the uterine cavity. This type of fibroid is considered a subtype of submucosal fibroids, which are fibroids that grow just beneath the lining of the uterus.
(e) Fibroid in Statu Nascendi
“Fibroid in statu nascendi” is a Latin term that translates to “fibroid in the process of forming” or “fibroid in the early stages of development.”
Fibroids in statu nascendi are generally not detectable through routine imaging studies such as ultrasound or MRI, as they are still in the early stages of development. They may not cause any symptoms, and their presence may only be suspected if a woman experiences symptoms such as heavy menstrual bleeding, pelvic pain, or pelvic pressure, and further evaluation is conducted.
It’s important to note that fibroids can grow and change over time, and even small fibroids in statu nascendi can potentially grow larger and cause symptoms in the future. Monitoring and follow-up with a healthcare provider may be recommended for women who are suspected to have fibroids in statu nascendi, especially if they start experiencing symptoms or if the fibroids are expected to potentially impact fertility or reproductive health.
(f) Intraligamental Fibroids
Intraligamental fibroids, also known as broad ligament fibroids, are a type of uterine fibroid that grows within the broad ligament of the uterus. The broad ligament is a fold of tissue that supports the uterus and connects it to the pelvic sidewall. Intraligamental fibroids are rare and account for only about 1-2% of all uterine fibroids.
Intraligamental fibroids are classified as subserosal fibroids, as they grow on the outside of the uterus and are covered by the peritoneum, which is the thin lining of the abdominal cavity. However, due to their location within the broad ligament, they may have a different presentation and characteristics compared to subserosal fibroids that grow on the surface of the uterus.
Causes of Fibroids
The exact cause of uterine fibroids is still unclear, but there are several factors that are believed to contribute to their development. These factors include:
- Genetic predisposition: There is evidence to suggest that there may be a genetic component to the development of fibroids. If a woman has a family history of fibroids, her risk of developing fibroids may be increased.
- Hormonal factors: Hormones, such as estrogen and progesterone, play a role in the growth and maintenance of the uterine lining during the menstrual cycle. It is believed that hormonal imbalances, such as an excess of estrogen relative to progesterone, may contribute to the development of fibroids. Estrogen promotes the growth of uterine lining, and progesterone counteracts estrogen’s effects. Therefore, an imbalance between estrogen and progesterone can lead to fibroid growth.
- Growth factors: Certain growth factors, such as insulin-like growth factor (IGF) and transforming growth factor-beta (TGF-beta), may also be involved in the development of fibroids. These growth factors can stimulate the growth of cells in the uterine wall, leading to the formation of fibroids.
- Race and ethnicity: Studies have shown that fibroids are more common in certain racial and ethnic groups, particularly in women of African descent. The reasons for this disparity are not fully understood and may involve a combination of genetic, hormonal, and environmental factors.
- Obesity: It’s worth noting that obesity, which is often associated with higher body fat levels, may indirectly affect the development of fibroids through hormonal imbalances. Adipose tissue, or fat cells, can produce estrogen, a female sex hormone that is known to play a role in the growth and maintenance of the uterine lining. An excess of estrogen in the body, which can occur in obese women due to increased production of estrogen by fat cells, may contribute to the development of fibroids or exacerbate existing fibroids.
- Other factors: Other factors that have been proposed as potential contributors to the development of fibroids include diet, lifestyle factors (such as stress and lack of exercise), and environmental factors (such as exposure to environmental toxins).
It’s important to note that fibroids are often the result of a combination of factors, and the exact cause may vary from woman to woman. The development of fibroids is a complex process that is still not fully understood, and research is ongoing to better understand the underlying causes and risk factors associated with fibroids.
Factors that Increase the Risk of Fibroids
There are several risk factors that have been associated with an increased likelihood of developing uterine fibroids. These risk factors include:
- Age: Fibroids are more commonly diagnosed in women of reproductive age, typically between the ages of 30 and 50. The risk of developing fibroids generally decreases after menopause.
- Family history: Having a close family member, such as a mother or sister, with a history of fibroids may increase a woman’s risk of developing fibroids. There may be a genetic component to the development of fibroids, although the exact genes involved are not yet fully understood.
- Race and ethnicity: Fibroids are more common in certain racial and ethnic groups, particularly in women of African descent. Studies have shown that women of African descent are more likely to develop fibroids at a younger age, have larger fibroids, and experience more severe symptoms compared to women of other races or ethnicities.
- Hormonal factors: Hormones, particularly estrogen and progesterone, play a role in the development of fibroids. Women with hormonal imbalances, such as an excess of estrogen relative to progesterone, may be at higher risk for developing fibroids.
- Reproductive history: Women who have never been pregnant or have had few or no pregnancies may have an increased risk of developing fibroids. Conversely, having multiple pregnancies and breastfeeding may lower the risk of fibroids.
- Obesity: There may be a link between obesity and an increased risk of fibroids. Excess body weight, particularly visceral fat around the abdomen, can increase estrogen levels in the body, which may contribute to the development of fibroids.
- Lifestyle factors: Certain lifestyle factors, such as a sedentary lifestyle, poor diet, and high stress levels, may also increase the risk of fibroids. Regular exercise, a healthy diet, and stress management techniques may help reduce the risk of fibroids.
- Other health conditions: Certain health conditions, such as polycystic ovary syndrome (PCOS) and metabolic syndrome, have been associated with an increased risk of fibroids.
It’s important to note that having one or more risk factors does not necessarily mean that a woman will develop fibroids, and many women with fibroids have no identifiable risk factors. The development of fibroids is likely influenced by a combination of multiple factors, and further research is needed to fully understand the complex mechanisms involved in fibroid development.
Can Fibroids Impact Pregnancy and Fertility?
Fibroids can impact pregnancy and fertility in some cases. Here are some ways in which fibroids can affect pregnancy and fertility:
- Difficulty in Conceiving: Large fibroids or fibroids located near the fallopian tubes or cervix can potentially interfere with conception by blocking the sperm’s access to the egg or preventing implantation of a fertilized egg in the uterus. Submucosal fibroids, which are located in the inner lining of the uterus, are particularly associated with fertility issues.
- Increased Risk of Miscarriage: Fibroids, especially submucosal fibroids, can increase the risk of early pregnancy loss or miscarriage. The presence of fibroids can disrupt the normal implantation process, leading to failed pregnancies.
- Uterine Distortion: Fibroids that grow inside the uterus can distort the shape and size of the uterine cavity, which can make it difficult for a fertilized egg to implant and establish a pregnancy. This can increase the risk of miscarriage and other pregnancy complications.
- Pregnancy Complications: Fibroids, particularly large fibroids, can increase the risk of various pregnancy complications such as preterm labor, premature rupture of membranes, placental abruption, and malpresentation of the baby. These complications can potentially impact the health of the mother and the baby during pregnancy.
- Impact on Fertility Treatments: Fibroids can also impact the success of fertility treatments such as in vitro fertilization (IVF) by affecting the implantation of embryos or the response to fertility medications. Fibroids may need to be treated or removed prior to undergoing fertility treatments to optimize the chances of success.
It’s important to note that not all fibroids are associated with infertility, and many women with fibroids are able to conceive and have successful pregnancies. The impact of fibroids on pregnancy and fertility can vary depending on the size, location, and number of fibroids, as well as the individual woman’s fertility factors.
Diagnosis of Fibroids
The diagnosis of fibroids typically involves a combination of medical history, physical examination, and imaging studies. Here are the common methods used for diagnosing fibroids:
- Medical History: A thorough medical history, including any symptoms related to fibroids, such as heavy menstrual bleeding, pelvic pain, or urinary symptoms, is usually taken to assess the possibility of fibroids.
- Physical Examination: A pelvic examination is typically performed to check for any abnormal growths or masses in the uterus or pelvis. Fibroids can sometimes be felt as firm, irregularly shaped masses during a pelvic examination.
- Imaging Studies: Imaging studies are commonly used to confirm the presence of fibroids and determine their size, number, and location. The following imaging modalities are commonly used:
- Ultrasound: Transvaginal or abdominal ultrasound is often the first imaging study performed to visualize the uterus and detect fibroids. Ultrasound can help determine the size, location, and number of fibroids, as well as their impact on the surrounding structures.
- Magnetic Resonance Imaging (MRI): MRI may be used in cases where ultrasound is inconclusive or to get more detailed information about the size, location, and characteristics of fibroids. MRI can provide clear images of the uterus and fibroids, helping to plan appropriate treatment options.
- Hysteroscopy: Hysteroscopy is a minimally invasive procedure that involves inserting a thin, flexible tube with a light and camera (hysteroscope) into the uterus through the cervix to directly visualize the inside of the uterus. This can be used to detect submucosal fibroids or other abnormalities in the uterine cavity.
- Biopsy: In some cases, a biopsy may be performed to rule out other conditions that may mimic fibroids, such as uterine cancer. A small tissue sample may be taken for examination under a microscope to confirm the presence of fibroids and rule out other conditions.
Once the diagnosis of fibroids is confirmed, additional tests may be performed as needed to assess the size, location, and impact of the fibroids on a woman’s overall health and fertility.
- Classification of Uterine Fibroids
- - Subserosal Fibroids
- - Intramural Fibroids
- - Submucosal Fibroids
- Causes of Fibroids
- Factors that Increase the Risk of Fibroids
- Can Fibroids Impact Pregnancy and Fertility?
- Diagnosis of Fibroids
- Surgical Methods for the Treatment of Fibroids
- - Myomectomy
- - Hysterectomy
- - Uterine Artery Embolization (UAE)
-
- MRI-Guided High-Intensity
Focused Ultrasound (MRgHIFU) - - Endometrial Ablation
-
- Laparoscopic or Robotic-Assisted
Fibroid Removal
Surgical Methods for the Treatment of Fibroids
There are several surgical methods that can be used for the treatment of fibroids, depending on the size, location, and symptoms associated with the fibroids, as well as the overall health of the patient. Here are some common surgical methods for fibroids
Myomectomy
Myomectomy is a surgical procedure that involves the removal of fibroids while preserving the uterus. It is typically recommended for women who wish to retain their fertility or have smaller fibroids that can be easily removed. Myomectomy can be performed via different techniques, including open abdominal surgery, laparoscopic surgery, or hysteroscopic surgery, depending on the size and location of the fibroids.
According to data from Healthcare Bluebook, the estimated average cost of myomectomy in the United States ranges from $6,000 to $12,000 for an abdominal myomectomy, $8,000 to $15,000 for a laparoscopic myomectomy, and $10,000 to $20,000 for a robotic-assisted myomectomy. Hysteroscopic myomectomy, which is typically less invasive, may have a lower average cost ranging from $3,000 to $8,000.
It’s recommended to request an appointment with New York Gynecology Endometriosis (NYGE) to obtain an accurate estimate of the cost.
Hysterectomy
Hysterectomy is a surgical procedure that involves the removal of the uterus, and sometimes the cervix, which eliminates the possibility of future pregnancies. Hysterectomy may be recommended for women who have large fibroids, severe symptoms, or do not wish to preserve their fertility.
Uterine Artery Embolization (UAE)
UAE is a minimally invasive procedure that involves blocking the blood supply to the fibroids, causing them to shrink and eventually die. It is performed by a radiologist using a catheter to inject tiny particles into the blood vessels that supply the fibroids, cutting off their blood flow.
MRI-Guided High-Intensity Focused Ultrasound (MRgHIFU):
MRgHIFU is a non-invasive procedure that uses high-intensity ultrasound waves to heat and destroy fibroid tissue while sparing the surrounding healthy tissue. It is guided by MRI imaging to precisely target and treat the fibroids.
Endometrial Ablation
Endometrial ablation is a minimally invasive procedure that involves the removal or destruction of the inner lining of the uterus (endometrium). It may be recommended for women with submucosal fibroids, which are located in the inner lining of the uterus, and cause heavy menstrual bleeding.
Laparoscopic or Robotic-Assisted Fibroid Removal
Laparoscopic or robotic-assisted surgery may be used for the removal of fibroids. These minimally invasive procedures involve small incisions and the use of specialized instruments to remove or shrink the fibroids.
Pankaj Singhal, MD, MS, MHCM
Master Surgeon in Robotic Surgery
Dr. Pankaj Singhal, a globally recognized endometriosis surgeon, possesses over 25 years of expertise in laparoscopic excision surgery, enabling him to tackle even the most challenging endometriosis cases with confidence. Dr. Pankaj treats patients with diverse endometriosis-related conditions, ranging from ovarian endometriomas to severe deep infiltrating endometriosis that affects the bowels and other organs.
Dr. Pankaj prioritizes minimally invasive surgery and provides comprehensive personal care. Additionally, he is the owner and founder of New York Gynecology and Endometriosis (NYGE), and has dedicated his life to advocating for, respecting, and treating women suffering from this little-known disease. He is one of the few surgeons in the entire United States who have completed over 5,718 robot-assisted gynecologic surgeries.

We Accept Most Major Insurance Plans
Convenient Billing Options for Comprehensive Coverage
Request an Appointment with
New York Gynecology Endometriosis
"*" indicates required fields